Rare diseases, defined in the U.S. as conditions affecting fewer than 200,000 people and in Europe as fewer than 1 in 2,000, comprise thousands of distinct disorders and affect millions globally.1 Though each is individually uncommon, together they impact a substantial population. Adherence to treatment is critical for favorable outcomes, yet patients with rare diseases face many unique challenges that shape their medication behavior.
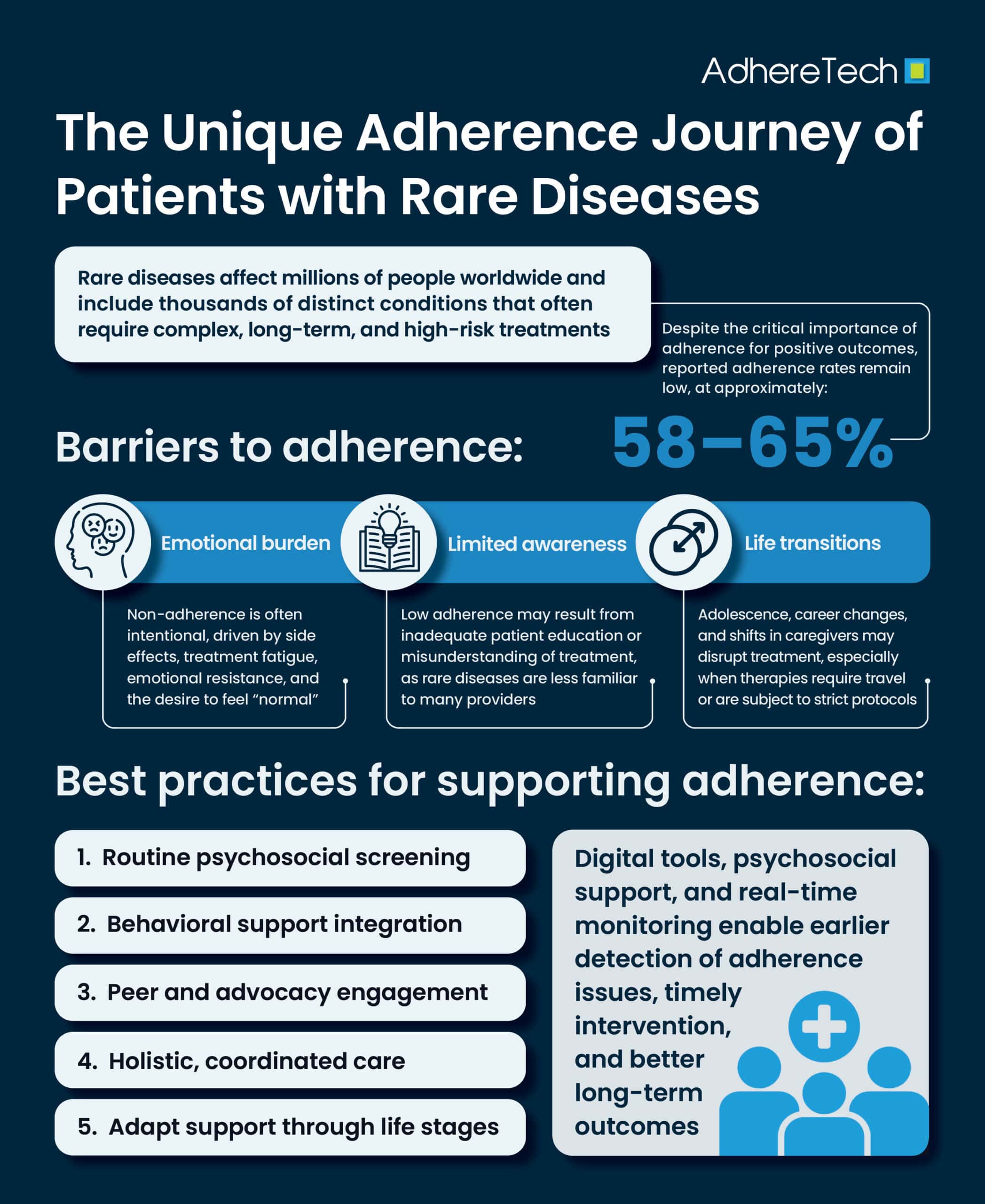
Treatments for rare diseases are high stakes and highly complex, involving long-term regimens with substantial side effects.² Drug therapies may require infusions, frequent dosing, or special transport and storage, making daily life more difficult and contributing to poor adherence—with reported rates ranging from 58–65%, among the highest for any chronic condition.³ Contrary to the common assumption that adherence failures are primarily due to forgetfulness, research shows that many patients with rare conditions deliberately stop treatment.⁴ A global study by Atlantis Health found that 55% wanted to “lead a normal life again,” 51% found constant medication inconvenient, and 49% wanted to see themselves as healthy. These findings suggest that patients may resist their diagnosis by rebelling against their treatment regimen, even while knowing its importance.² Resistance often increases after six to twelve months of treatment, when initial commitment can erode due to regimen fatigue, side effects, and the emotional burden of living with a rare disease.²
Low adherence can also result from inadequate patient education or misunderstanding of treatment.⁵ Rare diseases are less familiar to many healthcare providers; expertise may be limited, and guidelines may be unclear or inaccessible.⁶ As a result, patients and caregivers often assume the role of expert, striving to educate clinicians and navigate a fragmented healthcare landscape.⁷ The social dimension further compounds these challenges: rare disease patients and families frequently experience social isolation because their conditions are little known.⁸ Advocacy groups and peer platforms like RareConnect empower patients through connection, shared learning, and mutual support, reinforcing adherence by reducing stigma and offering practical guidance.⁸
For diseases diagnosed in childhood, the transfer of responsibility from caregiver to patient can disrupt adherence.⁹ Adolescents seeking independence may rebel, skip treatment, or hide their illness, particularly when peer acceptance feels at stake.10 In addition, logistical barriers such as access and cost play a significant role.11 Rare disease treatments are often expensive, specialized, and subject to strict reimbursement or approval protocols.11Travel burdens for infusions or monitoring visits and financial pressures can delay access and interrupt consistency.11
Digital and electronic tools are often leveraged to support adherence in rare disease contexts. Patient portals, digital companion programs, and smart bottles, provide objective tracking, feedback, and motivational prompts.12 Beyond technology, effective support must address psychological factors: non-adherence is often rooted in emotional resistance.13 Behavior change models like Acceptance and Commitment Therapy (ACT) help patients process their illness, align actions with personal values, and maintain treatment despite discomfort.14 Integrating psychosocial assessment tools into routine care ensures timely identification and intervention when resistance emerges.
For patients living with rare diseases, maintaining treatment adherence can be particularly challenging, especially when side effects or unexpected complications arise. If patients begin to drop off their prescribed therapies, early identification is crucial to prevent setbacks in care.15 Real-time monitoring plays a vital role in this process, allowing clinicians to quickly detect changes in adherence patterns or adverse reactions.16 By capturing data as it happens, care teams can intervene promptly—adjusting treatment plans, offering support, or managing side effects before they lead to full discontinuation. This timely response not only helps patients stay on therapy but also improves the overall likelihood of successful long-term outcomes.17
Ultimately, rare disease care benefits from integrated, multi-stakeholder support. Collaboration among specialists, pharmacies, social workers, payers, patient advocates, and digital solution providers is essential. IQVIA’s “Intelligent Interventions” approach illustrates how data-driven tracking and coordinated action across stakeholders can sustain adherence monitoring and response.18
The Journey in Phases
A typical rare disease adherence journey unfolds in stages:19
- Diagnosis and Education: Overcoming diagnostic “odyssey,” learning about condition and treatment, managing hope vs. fear.
- Early Treatment Engagement: Motivation is often high, but side effects and routine impact can emerge.
- Months 6–12: Burnout Phase: Regimen fatigue, emotional resistance, desire for normalcy often slow adherence
- Transition and Life Milestones: Adolescence, career changes, changes in caregivers may disrupt stability
- Long-Term Sustainability: Requires ongoing psychosocial support, reminders, access management, and periodic reengagement.
Best Practices for Supporting Adherence
1. Routine Psychosocial Screening20
Regularly assess for treatment fatigue, emotional resistance, or burnout. Administer short surveys during clinic visits or via patient apps to identify risk early.
2. Behavioral Support Integration17
Offer access to psychological therapies like ACT to assist in acceptance and resilience. These services should be standard, not an afterthought.
3. Peer and Advocacy Engagement21
Connect patients to communities like RareConnect or EURORDIS. Hearing from similar others reduces isolation, builds trust, and shares practical adherence tips
4. Holistic, Coordinated Care
Adherence support should involve multi-disciplinary teams: medical, behavioral, pharmacy, payer navigation—particularly for access and cost challenges.22
5. Adapt Support Through Life Stages
Offer specialized programming during adolescence, life transitions, or early burnout phases. Prepare caregivers and young adults for changing roles.23
Patients with rare diseases embark on a complex and emotionally charged medication journey—one that is shaped not just by forgetfulness, but by psychological resistance, limited provider knowledge, financial burdens, and profound fatigue. Recognizing the intentional nature of many non-adherence cases is the first step toward compassionate and effective support. This journey isn’t a solo one—it requires partners at every step: clinicians, caregivers, communities, and systems aligned to walk alongside patients, adapting support as life evolves.
References
- Atkins, Jenny C, and Christine R Padgett. “Living with a Rare Disease: Psychosocial Impacts for Parents and Family Members – a Systematic Review.” Journal of Child and Family Studies, vol. 33, 1 Feb. 2024, https://doi.org/10.1007/s10826-024-02790-6.
- Baryakova, Tsvetelina H., et al. “Overcoming Barriers to Patient Adherence: The Case for Developing Innovative Drug Delivery Systems.” Nature Reviews Drug Discovery, vol. 22, no. 22, 27 Mar. 2023, pp. 1–23, https://doi.org/10.1038/s41573-023-00670-0.
- Clarke, Joe T.R., et al. “Toward a Functional Definition of a “Rare Disease” for Regulatory Authorities and Funding Agencies.” Value in Health, vol. 17, no. 8, Dec. 2014, pp. 757–761, https://doi.org/10.1016/j.jval.2014.08.2672.
- Cribbs, Kristen A, et al. “Capturing Real‐World Rare Disease Patient Journeys: Are Current Methodologies Sufficient for Informed Healthcare Decisions?” Journal of Evaluation in Clinical Practice, vol. 31, no. 1, 1 Feb. 2025, https://doi.org/10.1111/jep.70010. Accessed 22 Feb. 2025.
- Dindo, Lilian, et al. “Acceptance and Commitment Therapy: A Transdiagnostic Behavioral Intervention for Mental Health and Medical Conditions.” Neurotherapeutics, vol. 14, no. 3, 2017, pp. 546–553, www.ncbi.nlm.nih.gov/pmc/articles/PMC5509623/, https://doi.org/10.1007/s13311-017-0521-3.
- Gadkari, Abhijit S, and Colleen A McHorney. “Unintentional Non-Adherence to Chronic Prescription Medications: How Unintentional Is It Really?” BMC Health Services Research, vol. 12, no. 1, 14 June 2012, https://doi.org/10.1186/1472-6963-12-98. Accessed 2 Dec. 2019.
- Haendel, Melissa, et al. “How Many Rare Diseases Are There?” Nature Reviews Drug Discovery, vol. 19, no. 2, 1 Feb. 2020, pp. 77–78, www.nature.com/articles/d41573-019-00180-y, https://doi.org/10.1038/d41573-019-00180-y.
- Haygarova, Iva, et al. “Assessment of Medication Adherence in Patients with Rare Diseases: A Systematic Review.” Pharmacia, vol. 71, 18 Dec. 2024, pp. 1–13, https://doi.org/10.3897/pharmacia.71.e135645. Accessed 31 Jan. 2025.
- Health, Atlantis. “The High Cost of Rare Disease Medication Nonadherence.” Atlantis Health, 15 June 2023, atlantishealth.com/uk/news-and-publications/the-high-cost-of-rare-disease-medication-nonadherence/. Accessed 19 Sept. 2025.
- “Intelligent Interventions: Guiding Rare Disease Patients along the Road of Adherence.” Https://Www.iqvia.com/Locations/United-States/Blogs/2022/10/Intelligent-Interventions-Guiding-Rare-Disease-Patients-Along-The-Road-of-Adherence, 2022, www.iqvia.com/locations/united-states/blogs/2022/10/intelligent-interventions-guiding-rare-disease-patients-along-the-road-of-adherence. Accessed 26 Sept. 2025.
- Macher, Marie-Alice, et al. “Transition of Care from Childhood and Adolescence to Adulthood in Nephrology.” Medecine Sciences : M/S, vol. 38, no. 2, Feb. 2022, pp. 182–190, pubmed.ncbi.nlm.nih.gov/35179473/, https://doi.org/10.1051/medsci/2022003.
- Mason, Madilyn, et al. “Technologies for Medication Adherence Monitoring and Technology Assessment Criteria: Narrative Review.” JMIR MHealth and UHealth, vol. 10, no. 3, 10 Mar. 2022, p. e35157, www.ncbi.nlm.nih.gov/pmc/articles/PMC8949687/, https://doi.org/10.2196/35157.
- “Mental Health & Wellbeing – EURORDIS-Rare Diseases Europe.” EURORDIS-Rare Diseases Europe, 29 July 2025, www.eurordis.org/mental-wellbeing/?utm. Accessed 19 Sept. 2025.
- Tsvetanov, Filip. “Integrating AI Technologies into Remote Monitoring Patient Systems.” Integrating AI Technologies into Remote Monitoring Patient Systems, vol. 37, 20 Aug. 2024, pp. 54–54, https://doi.org/10.3390/engproc2024070054.
- Uddin, Raihan, and Insoo Koo. “Real-Time Remote Patient Monitoring: A Review of Biosensors Integrated with Multi-Hop IoT Systems via Cloud Connectivity.” Applied Sciences, vol. 14, no. 5, 1 Jan. 2024, p. 1876, www.mdpi.com/2076-3417/14/5/1876, https://doi.org/10.3390/app14051876.
- Health (UK), National Collaborating Centre for Mental. DISCHARGE and TRANSFER of CARE. Www.ncbi.nlm.nih.gov, British Psychological Society, 2012, www.ncbi.nlm.nih.gov/books/NBK327301/.
- Sockalingam, Sanjeev, et al. “Identifying Opportunities to Improve Management of Autoimmune Hepatitis: Evaluation of Drug Adherence and Psychosocial Factors.” Journal of Hepatology, vol. 57, no. 6, Dec. 2012, pp. 1299–1304, https://doi.org/10.1016/j.jhep.2012.07.032. Accessed 26 Apr. 2022.
- Stenberg, Una, et al. “A Scoping Review of Health Literacy in Rare Disorders: Key Issues and Research Directions.” Orphanet Journal of Rare Diseases, vol. 19, no. 1, 6 Sept. 2024, https://doi.org/10.1186/s13023-024-03332-5.
- Taddeo, Danielle, et al. “Adherence to Treatment in Adolescents.” Paediatrics & Child Health, vol. 13, no. 1, 13 Jan. 2008, pp. 19–24, https://doi.org/10.1093/pch/13.1.19.
- Taibanguay, Nichapa, et al. “Effect of Patient Education on Medication Adherence of Patients with Rheumatoid Arthritis: A Randomized Controlled Trial.” Patient Preference and Adherence, vol. 13, no. 1, 11 Jan. 2019, pp. 119–129, www.ncbi.nlm.nih.gov/pmc/articles/PMC6333161/, https://doi.org/10.2147/ppa.s192008.
- Zhang, Huanyu, et al. “Physicians’ Knowledge on Specific Rare Diseases and Its Associated Factors: A National Cross-Sectional Study from China.” Orphanet Journal of Rare Diseases, vol. 17, no. 1, 5 Mar. 2022, https://doi.org/10.1186/s13023-022-02243-7.
- Pringle, Janice, and Kim Coley. “Improving Medication Adherence: A Framework for Community Pharmacy-Based Interventions.” Integrated Pharmacy Research and Practice, Nov. 2015, p. 175, https://doi.org/10.2147/iprp.s93036.
- Lockertsen, Veronica, et al. “The Transition Process between Child and Adolescent Mental Services and Adult Mental Health Services for Patients with Anorexia Nervosa: A Qualitative Study of the Parents’ Experiences.” Journal of Eating Disorders, vol. 9, no. 1, 13 Apr. 2021, https://doi.org/10.1186/s40337-021-00404-w.