Access to quality and equitable healthcare has been a challenge in remote and rural areas for centuries. But a powerful shift is underway, thanks to digital health technologies such as telemedicine, remote patient monitoring (RPM), and virtual clinical trials. These innovations are closing the gap in healthcare delivery, improving outcomes, and making care more accessible and efficient for millions of people who previously faced significant barriers.
What Is Telemedicine and Why Is It Crucial for Rural Health?
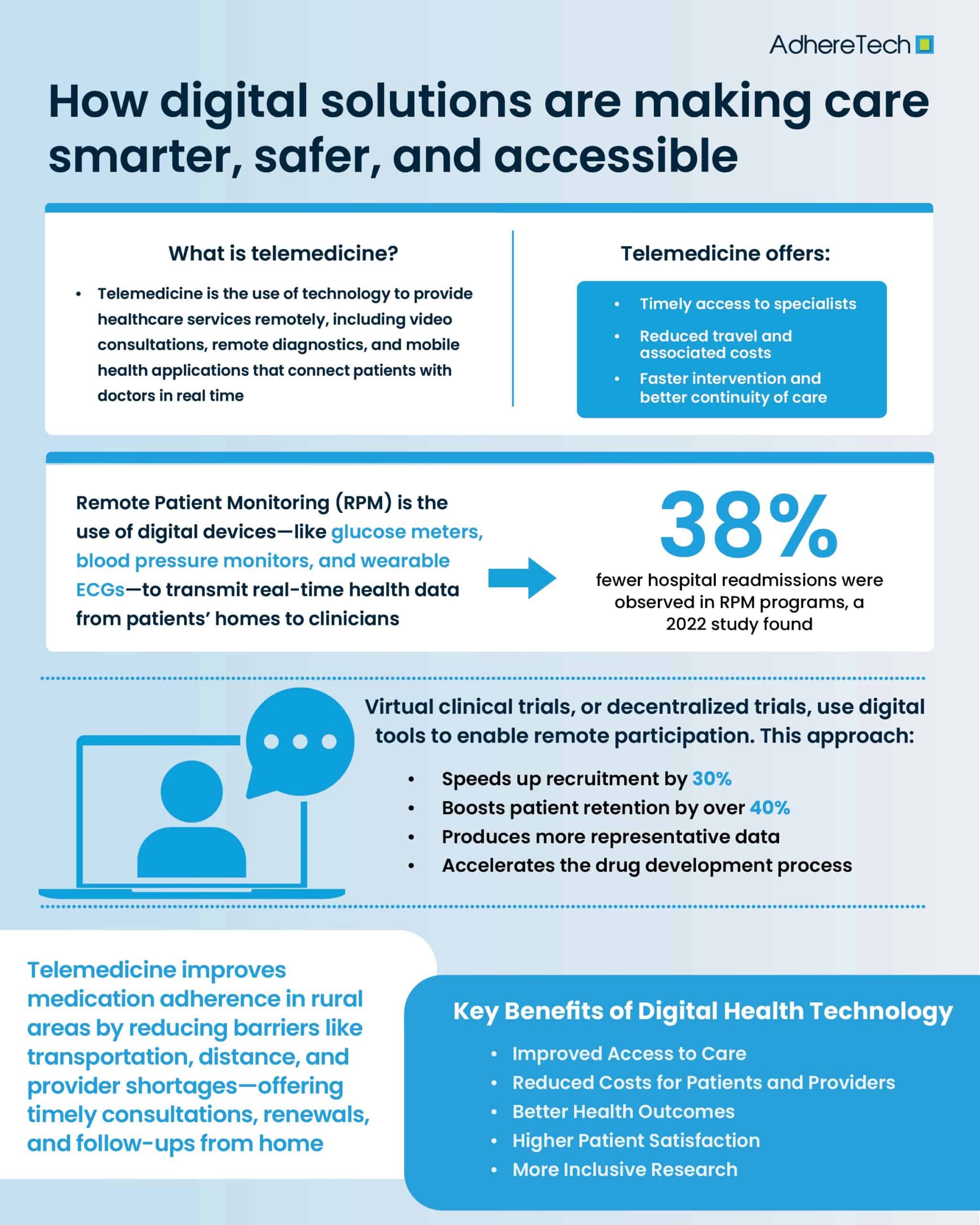
Telemedicine refers to the use of technology to provide healthcare services remotely, including video consultations, remote diagnostics, and mobile health applications that connect patients with doctors in real time from the comfort of their own home1.
For rural populations, where hospitals may be dozens or even hundreds of miles away, telemedicine is a lifeline. It offers timely access to specialists, reduced travel and associated costs, and faster intervention and better continuity of care1. According to the American Hospital Association (2021), more than 75% of U.S. hospitals now use telehealth to connect with patients2. In remote communities, this is helping to eliminate long-standing geographic barriers to care.
Remote Patient Monitoring: A New Era of Chronic Disease Management
RPM involves the use of digital devices to collect health data from patients in their homes3. Common RPM tools include blood pressure monitors, glucose meters, pulse oximeters, smartwatches, and wearable ECGs3.
These devices transmit real-time data to healthcare providers, who can intervene quickly if readings fall outside of normal ranges3. This is especially critical for patients managing chronic diseases such as diabetes, hypertension, and heart failure—conditions that are more prevalent in rural communities4. A 2022 study in the Journal of Medical Internet Research found that RPM programs reduced hospital readmissions by 38% and improved medication adherence among chronic disease patients5.
In underserved areas with limited provider access, RPM empowers clinicians to deliver continuous care, improving both outcomes and patient engagement.
Virtual Clinical Trials: Expanding Access to Cutting-Edge Treatments
Virtual clinical trials, also known as decentralized clinical trials, use digital platforms and mobile technologies to conduct research without requiring participants to travel to study sites6. This approach offers enormous potential to rural and underserved populations, who have traditionally been underrepresented in clinical research due to their geographic isolation, transportation challenges, and time and financial constraints6.
By using tools like telemedicine, mobile apps, home sample collection kits, and wearable devices, virtual trials allow for remote participation, better diversity, and higher retention rates. A 2023 report from Clinical Trials Arena noted that decentralized trials reduced recruitment times by 30% and increased participant retention by over 40%7.
This model not only speeds up the drug development process but also ensures that research findings are more representative of real-world populations.
Key Benefits of Digital Health Technology in Remote Communities
The integration of telemedicine, RPM, and virtual trials is more than just a technological upgrade—it’s a positive shift in how healthcare is delivered, especially in underserved areas.
1. Improved Access to Care: Digital tools eliminate the need for long-distance travel and the associated costs, as well as provide access to specialists not available locally8.
2. Reduced Costs for Patients and Providers: Telehealth and remote monitoring reduce the likelihood and burden of emergency visits, hospital stays, and transportation costs9.
3. Better Health Outcomes: Regular monitoring and early intervention lead to improved management of chronic diseases and fewer long-term complications10.
4. Higher Patient Satisfaction: Patients value the convenience and responsiveness of digital care, particularly those managing ongoing conditions11.
5. More Inclusive Research: Virtual clinical trials help life-saving research reach populations who would otherwise be excluded12.
Challenges of Digital Health in Rural Areas: Barriers to Equitable Access and Adoption
While digital health holds immense promise, several barriers must be addressed to ensure equitable adoption in remote regions. Firstly, limited broadband access. According to the FCC, over 14 million Americans in rural areas still lack reliable high-speed internet13. Secondly, some populations, especially older adults, may struggle with navigating telehealth platforms, and finally, there are many privacy and security concerns that come with digital healthcare, considering the sensitive nature of the data they collect.
Policy Recommendations and Future Outlook
To fully realize the benefits of digital health technologies, governments, healthcare organizations, and tech providers must work together to increase the accessibility of digital health and telemedicine to rural populations. This may entail designing inclusive platforms that do not require high speed wifi, investing in training programs to increase digital literacy among both patients and providers, and ensuring data protection and interoperability across platforms.
How Telemedicine Enhances Medication Adherence in Rural Communities
Telemedicine plays a critical role in improving medication adherence among patients in rural areas by bridging gaps in healthcare access and continuity. The challenges of limited transportation, long distances to clinics, and shortages of healthcare providers can all contribute to missed appointments and poor medication management. With telemedicine, patients can receive timely consultations, prescription renewals, and follow-ups from the comfort of their homes, reducing these barriers significantly. Furthermore, digital health platforms often include medication reminders, educational content, and virtual support, which foster better understanding and commitment to prescribed treatments. Studies have shown that due to increased accessibility, telehealth interventions can lead to improved medication adherence, particularly in chronic disease management14. By ensuring regular engagement with healthcare professionals, telemedicine empowers rural patients to take a more active role in their health, leading to better outcomes and reduced hospitalizations.
As investments in digital health infrastructure and policy continue to grow, the future of rural healthcare looks increasingly connected—and far more hopeful.
References
- Mayo Clinic. “Telehealth: Technology Meets Health Care.” Mayo Clinic, 5 Sept. 2024, www.mayoclinic.org/healthy-lifestyle/consumer-health/in-depth/telehealth/art-20044878.
- American Hospital Association. (2021). Telehealth: A Path to Virtual Integrated Care. https://www.aha.org
- Claggett, Jennifer. “An Infrastructure Framework for Remote Patient Monitoring Interventions and Research (Preprint).” JMIR. Journal of Medical Internet Research/Journal of Medical Internet Research, vol. 26, 30 May 2024, pp. e51234–e51234, https://doi.org/10.2196/51234.
- Ramesh, Jeevitha, et al. “The Impact of Chronic Diseases on Cognitive Impairment in Rural Population of India: A Focus on Diabetes, Hypertension, Cardiovascular Disease, and Stroke.” Brain Behavior and Immunity Integrative, 1 Feb. 2025, pp. 100107–100107, https://doi.org/10.1016/j.bbii.2025.100107.
- Journal of Medical Internet Research. (2022). Remote Monitoring and Chronic Disease Management. https://www.jmir.org
- Yared Santa-Ana-Tellez, et al. Decentralised, Patient-Centric, Site-Less, Virtual, and Digital Clinical Trials? From Confusion to Consensus. Vol. 28, no. 4, 1 Feb. 2023, pp. 103520–103520, https://doi.org/10.1016/j.drudis.2023.103520.
- Clinical Trials Arena. (2023). Decentralized Clinical Trials: Market Trends and Patient Inclusion. https://www.clinicaltrialsarena.com
- GlobalData UK Ltd. “Remote Patient Monitoring Will Continue to Transform Healthcare Delivery and Clinical Trials in 2021.” GlobalData, GlobalData UK Ltd., 19 Jan. 2021, www.globaldata.com/media/pharma/remote-patient-monitoring-will-continue-transform-healthcare-delivery-clinical-trials-2021/. Accessed 19 May 2025.
- Mudiyanselage, Shalika Bohingamu , et al. “Cost-Effectiveness of Personalised Telehealth Intervention for Chronic Disease Management: A Pilot Randomised Controlled Trial.” PLOS One, vol. 18, no. 6, 15 June 2023, pp. e0286533–e0286533, https://doi.org/10.1371/journal.pone.0286533.
- Handelsman, Yehuda, et al. “Early Intervention and Intensive Management of Patients with Diabetes, Cardiorenal, and Metabolic Diseases.” Journal of Diabetes and Its Complications, vol. 37, no. 2, 1 Jan. 2023, pp. 108389–108389, https://doi.org/10.1016/j.jdiacomp.2022.108389.
- Madanian, Samaneh , et al. “Patients’ Perspectives on Digital Health Tools.” PEC Innovation, vol. 2, no. 2, 1 May 2023, pp. 100171–100171, https://doi.org/10.1016/j.pecinn.2023.100171.
- Goodson, Noah, et al. “Opportunities and Counterintuitive Challenges for Decentralized Clinical Trials to Broaden Participant Inclusion.” Npj Digital Medicine, vol. 5, no. 1, 5 May 2022, https://doi.org/10.1038/s41746-022-00603-y.
- Federal Communications Commission (FCC). (2022). Broadband Deployment Report.
- Kruse, C. S.,et al. (2018). Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open, 7(8), e016242. https://doi.org/10.1136/bmjopen-2017-016242