November marks National Care at Home month, a time dedicated to ensuring all patients have access to “high-quality, person-centered healthcare where they call home.”1
Receiving care from the comfort of one’s own home is more than just a convenience, it offers profound benefits – increased independence, enhanced quality of life, and emotional stability.2 Each of these factors are essential for prompting successful recovery and long-term physical and mental wellness.2
Home care enables patients to heal within familial, supportive environments where personalized care and dignity remain at the forefront of every individual’s treatment plan. Unlike hospitals and clinical care facilities, where individualized attention is often diluted due to institutional routines and high provider to patient volumes, home care ensures the continuity of care through one-on-one support tailored to patient’s evolving needs.2
Whether such services are delivered to aging adults, children with complex medical needs, or individuals attempting manage chronic conditions, home-based care offers a care model that seeks to meet patients where they are, both emotionally and physically.2
The Benefits of Home-Based Care Over Hospitalization/Clinical Settings (when deemed appropriate)
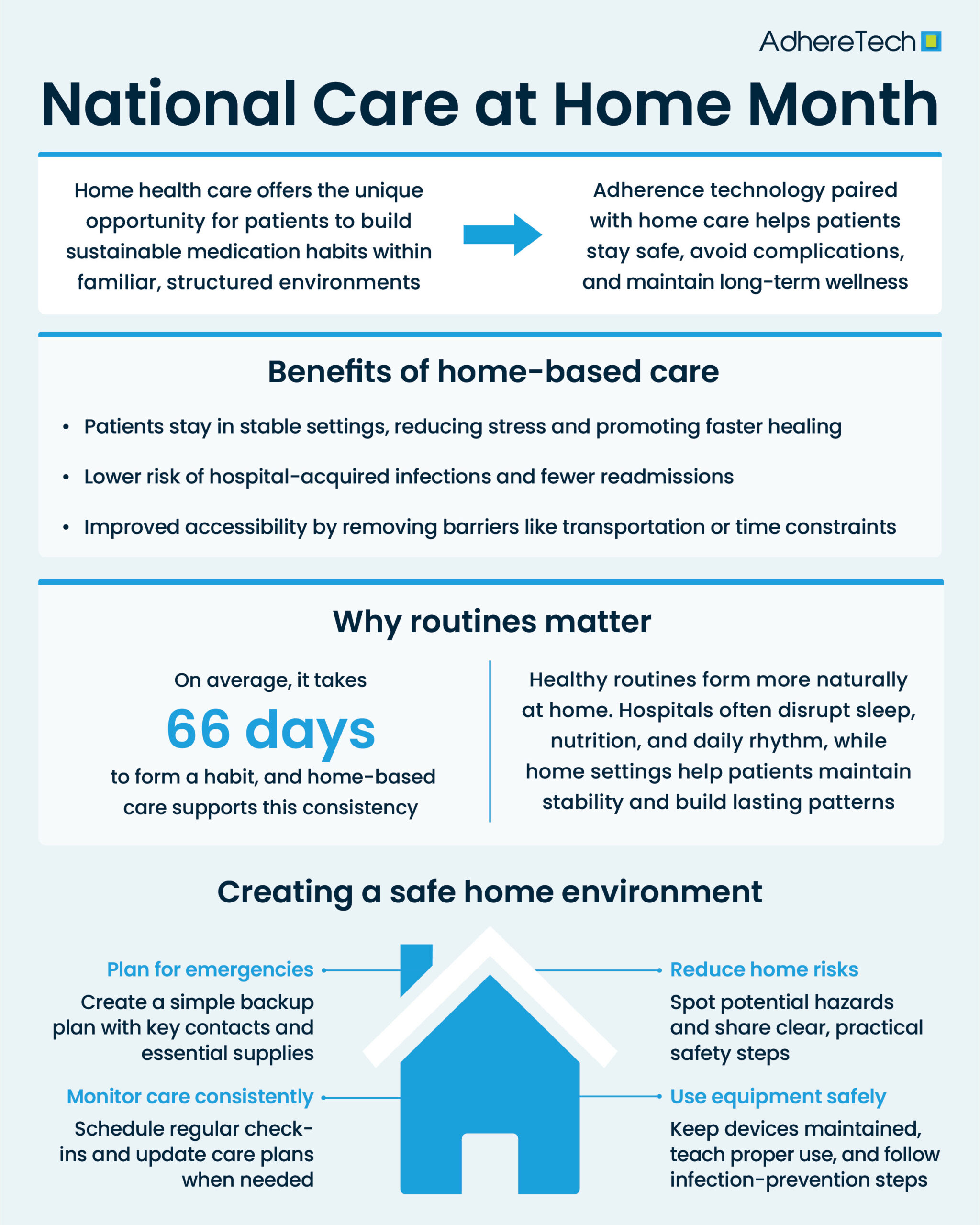
The predominant reason for home health care’s efficacy is that it allows patients to remain within a familiar setting, a context which facilitates maintenance of everyday routines and support from loved ones.3, 4 This emotional and environmental support has been associated with enhancements in emotional well-being and improvements in recovery outcomes,2 as patients experience greater comfort, reduced stress, and a stronger sense of control over their healing process. Moreover, the ability to personalize care within one’s home fosters greater adherence to treatment plans and sustained behavioral changes that contribute to long-term health.3, 5
Notably, research has found that patients who received “hospital-at-home” services had shorter length of stay, fewer readmissions, and better clinical outcomes when compared to patients residing within a true hospital setting.6 Such finding is of particular importance for patients who are immunocompromised, making them highly susceptible to the broad-spectrum of hospital acquired-infections, like norovirus, urinary tract, respiratory, blood, etc.2 Even when hospital safety protocols are followed stringently, the close proximity of patients within and volume of infectious diseases within clinical settings, can result in at-risk patients acquiring these acute conditions, further complicating their care and recovery.7
Extending beyond physical safety, home-based care can reinforce a sense of control and autonomy within patients, both components which are vital for adherence and long-term management of care. Patients can engage more actively within their own recovery, without the extensive oversight and limitations imposed within a clinical setting.2 Home care allows patients to remain close to their friends and family facilitating improved psychological well-being, a source of stimulations often lacking within clinical settings with rigid and limited visiting hours. Moreover, patients can maintain their daily routines and hobbies while simultaneously receiving individualized, empathetic support that extends beyond that offered within a clinical setting (likely due to practitioners seeing less patients and spending more time with individual patients).7
Home-based health services also have the opportunity to dramatically reduce healthcare costs and increase accessibility to services.8 Long travel times, lack of transportation, inability to take time off of work, child or elder care responsibilities, or difficulty with leaving one’s home are all potential barriers for patients receiving care in clinical settings.8 Home-based care services eliminate these barriers, bringing care directly to patients, reinforcing its patient-centricity.
Habit Formation: How Home-Based Care Supports Routines & Long-Term Habit Formation
Routine plays a critical role in supporting both physical and mental well-being, and establishing a consistent daily structure can help to create a sense of normalcy, alleviate anxiety, and support patients’ ability to manage their health more effectively.9, 10
Hospitalization and long-term stays within clinical settings place patients in an unfamiliar environment that disrupts their established daily routines.11 Patients’ familiar surroundings, sleeping patterns, and daily habits are all dictated by institutional schedules as opposed to each individual patient’s established rhythms.11 Research highlights that patients in hospital-like settings frequently experience additional stressors on a regular basis, such as sleep deprivation and malnutrition.12
For example, reports suggest that malnutrition affects up to half of all hospitalized patients, which can result in severe consequences – “chronic inflammatory processes, muscle breakdown and organ damage.”12 Despite evidence highlighting that lack of proper nutrition’s association with longer hospital stays, mortality, and increased risk of adverse events, patients still rarely receive comprehensive nutritional consults.12 Moreover, hospitals are notorious for serving poor-quality, low nutrient-density foods to minimize costs.12
Similarly, the often noisy and disruptive environments of hospitals,12 can prevent patients from getting the necessary rest they need to support their recovery. Despite the World Health Organization recommending that noise levels be kept below 35dB at night and 40 dB during the day, recent studies suggest noise levels in hospitals are greater than 55dB 70-90% of the time.12 Similarly, excessive collection of vital signs for low-risk patients may further disrupt sleep.12 For compromised patients, the consequences from sleep deprivation and malnutrition are often further amplified, and in combination with the stress resulting from their underlying condition(s), can lead to or worsen complications.12
Rush periods, severe cases, and staffing shortages can all cause further disruptions, creating an inconsistent and often stressful routine. For many, these additional disruptions can heighten stress, disorientation, and even lead to hospital associated delirium, a temporary condition marked by limited attention, incoherence, and poor cognition.13 Resultantly, re-establishing a stable rhythm once patients return to their natural home environment can be exceedingly challenging, especially when considering that many patients have become accustomed to having many aspects of care automatically managed for them by providers. Furthermore, patient surveys indicate significant inconsistencies when transitioning from clinical to home settings—confusion, gaps in care, lack of adequate resources, and poor information transfer between providers and patients upon discharge14 – all present additional barriers to patients’ ability to succeed in building and sustaining effective daily health routines.
In contrast, home-based care enables patients to preserve their daily rhythms and sense of independence without disruption. Within the comfort of their own homes, they can integrate medication routines, dietary habits, and physical or cognitive activities more naturally into everyday life. On average, it takes about 66 days to form a habit, underscoring the importance of stability and environmental consistency in sustaining positive health behaviors.15 Engaging in such behaviors at home reinforces autonomy and fosters a greater sense of control over one’s recovery, supporting better treatment adherence and long-term outcomes.
Research consistently shows that maintaining predictable routines supports improvements in sleep, mood, and overall mental health.¹ Stability in the home environment can also reduce confusion or disorientation among older adults or individuals living with chronic conditions, enabling them to focus more effectively on recovery and wellness.
By supporting patients in developing and maintaining healthy routines, home health care not only improves clinical outcomes but also enhances overall quality of life—empowering individuals to live more independently, confidently, and sustainably.
Research has shown that maintaining predictable routines can lead to improvements in sleep, mood, and overall mental health.10 Stability in the home environment can also reduce confusion or disorientation among older adults or individuals living with chronic conditions, enabling them to focus more effectively on recovery and wellness.
By supporting patients in developing and maintaining healthy routines, home health care not only improves clinical outcomes but also enhances overall quality of life,empowering individuals to live more independently, confidently, and sustainably.
Recommendations for Facilitating a Safe Home Environment that Promotes Patient Safety and Well-Being
Home-based care offers patients the comfort of receiving medical attention in their own homes while maintaining their independence and daily routines.16 However, the benefits of home care can only be fully realized when their home environments facilitate their safety, mitigating both potential and real hazards.16 Recommendations for ensuring a safe home environment include the following:
- Risk Assessment and Environment Safety: Home-based care providers should conduct thorough home safety assessments, evaluating hazards like uneven flooring, poor lighting, and unsafe equipment.16 Recommendations should be provided to patients and caregivers for minimizing any identified risks to ensure patient safety.16
- Medical Equipment and Infection Control: Providers must seek to ensure that medical equipment within patient’s homes is properly maintained, and infection prevention protocols are followed rigorously, protecting vulnerable patients from additional complications.16 Furthermore, providers should seek to provide training to patients and caregivers on the correct usage of medical equipment, and ensure awareness of appropriate procedures for reporting equipment malfunctions or potential signs of infection.16
- Emergency Preparedness: Given home-based care’s emphasis on patient-centered care, each patient should be provided with an individualized emergency plan that clearly outlines actions to be taken during the event of an emergency.16 These plans should be explained to patients and caregivers using plain language and patient/caregiver comprehension should be ensured by providers.16
Key components of emergency plans include the following:
- Contact information for emergency services, healthcare providers, and caregivers.16
- Readily available and easy accessibility of emergency supplies, such as first aid kits, additional medications, etc.16
- Medical alert devices that allow for immediate contact to emergency services.16
- Psychological and Social Well-Being: Ensuring the emotional and mental well-being of patients is just as important as their physical well-being.16 Strategies to promote social interactions, accessibility to mental health services, and ensuring supportive, stimulating environments for patients receiving care within their own homes is essential for enhancing their overall well-being and quality of life.16
- Medication Management: Proper medication administration and management is a vital component for ensuring patient safety and supporting their long-term well-being.16 Providing consistent and sustained access to medications, easy to follow medication dosing instructions, and patient and caregiver education on the importance of medication is essential for ensuring patients take their medications as prescribed, protecting their safety and increasing the likelihood of successful recovery.16
- Continuous Monitoring and Evaluation: For effective home-based care, individualized care plans should address a patient’s medical, physical, and emotional needs.16 Effective and continuous communication between care providers, patients, family members, and caregivers is essential for ensuring patient safety.16
- Regular check-ins, clear methods for real-time communication, and consistent evaluations of patient’s home and well-being should be conducted.16
The Importance of Medication Adherence in Home-health
One of the most significant drivers of successful home-based care is medication adherence.16 Each year, nonadherence contributes to over 125,000 preventable deaths and hundreds of billions in avoidable healthcare costs.17 It also increases the likelihood of hospital admissions and has consistently been associated with long-term health outcomes.17, 18 While the economic costs and structural strain imposed on the healthcare system are significant issues resulting from nonadherence, the costs associated with patients’ health and lives are undefinable.
While clinical settings provide continuous access to medication, often taken under provider supervision, they fail to support the formation of consistent medication-taking behaviors and long-term habits once patients transition from the facility. Hospital environments often revolve around staffing schedules, rounding times, and structured routines as opposed to individual patient needs. Medications are administered at prescribed times by staff,19 which prevents patients from having the opportunity to actively engage within their own care routines. This can create challenges in maintaining adherence once patients return to their own home environments. While some home-based care services offer similar monitoring services over patient’s medication, patients and/or their caregivers are often required to manage the dosing, timing, and consumption of patients’ medications.20
In contrast, home health care offers the unique opportunity for patients to build sustainable medication habits within familiar, structured environments.2 Patients can integrate their medication routines into their daily lives, such as alongside their meals, sleep schedules, or other personal habits. Over time, the consistency of such behavior can result in the formation of an association between medication and existing, established behaviors, facilitating the habit formation process.21 This continuity enables patients to learn, practice, and establish adherence behaviors in a context that aligns with their own lifestyle and rhythms.
For instance, a patient who receives their medication in the morning within a clinical setting may struggle to maintain that dosing schedule once they return to their daily routines. Work demands, childcare responsibilities, or simple forgetfulness can make their original dosing window difficult or impossible to follow.22, 23 However, in a home setting, medication timing can be aligned with the patient’s natural routines, making adherence easier and more sustainable. Digital adherence tools, such as AdhereTech’s smart devices, which offer customizable dosing windows, can provide an additional level of support and accountability for patients, by seamlessly integrating within their existing routines while monitoring adherence behaviors in real time.
For patients who require precise timing of their medications, even small deviations can reduce effectiveness or increase the risk of side effects.24 Digital adherence tools, like AdhereTech, are designed to facilitate this home-based care structure while simultaneously ensuring the safety of patients through real-time adherence monitoring. AdhereTech’s customizable devices passively monitor adherence, send timely and encouraging reminders, and provide real-time adherence data to patients, caregivers, and specialty pharmacies. Furthermore, the devices functionality via the cellular network and compatibility with all phone types helps to reduce gaps in the accessibility of home based healthcare for underserved patient populations.
By combining the supportive environment of home health care with digital adherence tools, patients gain both structure and autonomy. They are empowered to take an active role in their treatment, while providers and caregivers receive actionable insights to intervene proactively if challenges arise. This approach not only reduces the risk of missed doses or incorrect timing but also strengthens long-term adherence habits, ultimately improving health outcomes, reducing hospital readmissions, and enhancing patients’ overall quality of life.
Adherence technology, when paired with effective home-based care, ensures that patients not only remain safe but also stay on track with their treatments – preventing avoidable complications and supporting long-term wellness. As we celebrate National Care at Home Month, it serves as a reminder that care, safety, and adherence are most effective when delivered in environments where patients retain their autonomy, feel supported, and are able to maintain routines that work for them – something only home-based care can consistently provide.
References
1 National Alliance for Care at Home. (2025). National care at home month. https://allianceforcareathome.org/newsroom/national-care-at-home-month/
2 Atlantic Care Services. (2025, July 24). Why is home health care important? Atlantic Care Services. https://www.atlanticcareservices.com/why-is-home-health-care-important/ (atlanticcareservices.com)
3 Torres, P., Stoeppel, S. M., Young, J., Kiesel, J., Eberman, L. E., & Rivera, M. J. (2025). Therapeutic Alliance: Exploring the Patient-Clinician Relationship through the Experiences of Collegiate Student-Athletes with Athletic Trainers. Internet Journal of Allied Health Sciences and Practice, 23(2), 8.
4 Heart To Heart Healthcare. (2025, March 14). The impact of home care on family dynamics. https://www.h2hhc.com/blog/the-impact-of-home-care-on-family-dynamics
5 Opland, C., & Torrico, T. J. (2024). Psychotherapy and Therapeutic Relationship. In StatPearls [Internet]. StatPearls Publishing.
6 Kanagala, S. G., Gupta, V., Kumawat, S., Anamika, F., McGillen, B., & Jain, R. (2023). Hospital at home: emergence of a high-value model of care delivery. The Egyptian journal of internal medicine, 35(1), 21. https://doi.org/10.1186/s43162-023-00206-3
7 Mass General Brigham. (2024, July 11). Research shows inpatient hospital care at home is successful. https://www.massgeneralbrigham.org/en/about/newsroom/articles/research-shows-inpatient-hospital-care-at-home-is-successful/ (massgeneralbrigham.org)
8 O’Dell, M., & Wheeler, L. M. (2012). Home health care: healing where the heart is. Missouri medicine, 109(6), 439–442.
9 Cepni, A. B., Kirschmann, J. M., Rodriguez, A., & Johnston, C. A. (2025). When Routines Break: The Health Implications of Disrupted Daily Life. American Journal of Lifestyle Medicine, 15598276251381626.
10 Northwestern Medicine. (2022, December). Health benefits of having a routine: Tips for a healthier lifestyle. https://www.nm.org/healthbeat/healthy-tips/health-benefits-of-having-a-routine
11 HumanCare NY. (2025, March 27). The importance of establishing a routine in home care. https://www.humancareny.com/blog/the-importance-of-establishing-a-routine-in-home-care/
12 Xu, T., Wick, E. C., & Makary, M. A. (2016). Sleep deprivation and starvation in hospitalised patients: how medical care can harm patients. BMJ Quality & Safety, 25(5), 311-314.
13 Collier R. (2012). Hospital-induced delirium hits hard. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne, 184(1), 23–24. https://doi.org/10.1503/cmaj.109-4069
14 Jones, B., James, P., Vijayasiri, G., Li, Y., Bozaan, D., Okammor, N., … & Jenq, G. (2022). Patient perspectives on care transitions from hospital to home. JAMA network open, 5(5), e2210774-e2210774.
15 Frothingham, S. (2025, October 16). How long does it take for a new behavior to become a habit? Healthline. https://www.healthline.com/health/how-long-does-it-take-to-form-a-habit (healthline.com)
16 Kennedy, J., & Skehan, K. (n.d.). Home‑based patient care safety. Community Health Accreditation Partner. https://www.chapinc.org/blog-news/home-based-patient-care-safety/ (chapinc.org)
17 Benjamin, R. M. (2012). Medication adherence: helping patients take their medicines as directed. Public health reports, 127(1), 2-3.
18 Kvarnström, K., Westerholm, A., Airaksinen, M., & Liira, H. (2021). Factors Contributing to Medication Adherence in Patients with a Chronic Condition: A Scoping Review of Qualitative Research. Pharmaceutics, 13(7), 1100. https://doi.org/10.3390/pharmaceutics13071100
19 University of Connecticut John Dempsey Hospital. (2016, March). Commonly used standard times of administration (STOA). https://health.uconn.edu/pharmacy/wp-content/uploads/sites/60/2016/03/commonly_used_standard_times_of_administration.pdf
20 Johns Hopkins Medicine. (n.d.). Medication management and safety tips. https://www.hopkinsmedicine.org/health/wellness-and-prevention/help-for-managing-multiple-medications (hopkinsmedicine.org)
21 Ghai, I., Palimaru, A., Ebinger, J. E., Barajas, D., Vallejo, R., Morales, M., & Linnemayr, S. (2024). Barriers and facilitators of habit building for long-term adherence to antihypertensive therapy among people with hypertensive disorders in Los Angeles, California: a qualitative study. BMJ open, 14(7), e079401.
22 Chardon, M. L., Klages, K. L., Joffe, N. E., & Pai, A. L. H. (2022). Caregivers’ Experience of Medication Adherence Barriers during Pediatric Hematopoietic Stem Cell Transplant: A Qualitative Study. Journal of pediatric psychology, 47(6), 685–695. https://doi.org/10.1093/jpepsy/jsab138
23 Baryakova, T. H., Pogostin, B. H., Langer, R., & McHugh, K. J. (2023). Overcoming barriers to patient adherence: the case for developing innovative drug delivery systems. Nature reviews. Drug discovery, 22(5), 387–409. https://doi.org/10.1038/s41573-023-00670-0
24 Nagar, S., & Davey, N. (2015). Reducing avoidable time delays in immediate medication administration – learning from a failed intervention. BMJ quality improvement reports, 4(1), u206468.w2612. https://doi.org/10.1136/bmjquality.u206468.w2612