In recent years, personalized medicine has made significant strides in the field of healthcare, offering more tailored treatment plans that align with individual genetic profiles, lifestyles, and health conditions1. With this shift towards personalized healthcare, there’s been increasing recognition of the importance of ensuring patients adhere to prescribed treatments. Despite such recognition, medication nonadherence, which refers to patients failing to follow prescribed medication regimens, remains a critical issue that can seriously compromise treatment outcomes2.
What is Personalized Medicine
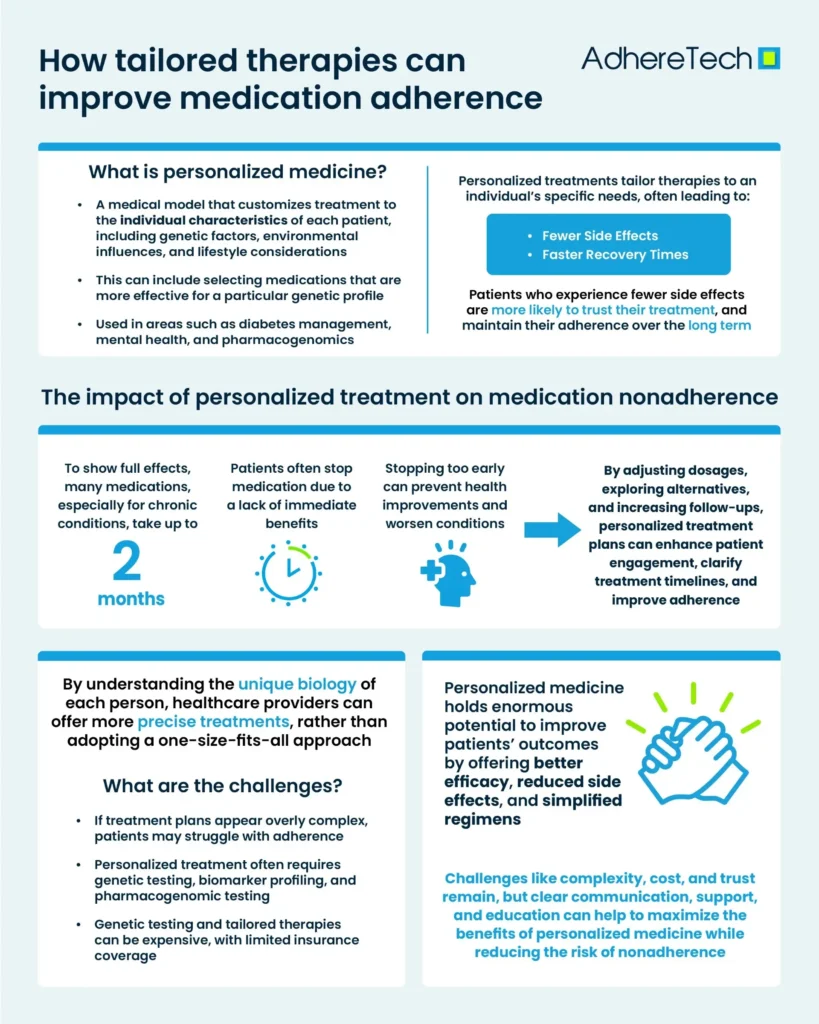
Personalized medicine, also known as precision medicine, is a medical model that tailors treatment to the individual characteristics of each patient1. This can include genetic factors, environmental influences, and lifestyle considerations1. The idea is that by understanding the unique biology of each person, healthcare providers can offer more precise treatments, rather than adopting a one-size-fits-all approach. Personalized medicine is also increasingly being used in areas such as diabetes management, mental health, and pharmacogenomics (the study of how genes affect a person’s response to drugs)3.
What Are The Benefits of Personalized Medicine in Medication Adherence
Although personalized medicine can simplify regimens in some cases, it can also lead to increased complexity in others; genetic testing, biomarker profiling, and pharmacogenomic testing are often required to personalize treatment6. This can involve a lengthy and sometimes confusing process for patients, particularly if they lack a clear understanding of the tests or their significance. If the treatment plan appears overly complex or difficult to follow, patients may struggle with adherence. Furthermore, personalized medicine, particularly genetic testing and tailored therapies, can also be expensive7, and in many cases, these treatments may not be covered by insurance, or the cost might be prohibitive for some patients. The high costs associated with such treatments can lead to financial stress, causing patients to stop taking their medications as prescribed8.
How Personalized Medicine Can Address Medication Nonadherence
One of the main reasons for medication nonadherence is that patients often don’t perceive any immediate benefit from their treatment9, leading them to stop taking the medication. This is particularly problematic because many medications, especially those for chronic conditions, can take up to two months of consistent use before their full benefits are felt10. When patients discontinue their medication too early, they miss out on potential improvements in their health, which can exacerbate their condition. A solution to this issue could lie in personalized treatments, where healthcare providers tailor medication plans to individual patients based on their specific needs, responses, and preferences. By adjusting dosages, exploring alternative medications, or offering more frequent follow-ups, personalized treatment plans can help patients feel more engaged in their treatment, better understand the timeline for potential benefits, and ultimately improve medication adherence.
Personalized medicine holds enormous potential to improve patient outcomes by tailoring treatments to the individual. When it comes to medication adherence, personalized regimes can offer significant benefits, including better efficacy, reduced side effects, and simplified regimens. However, challenges such as complexity, cost, and patient trust still need to be addressed. By focusing on clear communication, patient support, and education, the healthcare industry can maximize the benefits of personalized medicine while reducing the risk of nonadherence.
References
- Goetz, Laura H., and Nicholas J. Schork. “Personalized Medicine: Motivation, Challenges, and Progress.” Fertility and Sterility, vol. 109, no. 6, June 2018, pp. 952–963, www.ncbi.nlm.nih.gov/pmc/articles/PMC6366451/, https://doi.org/10.1016/j.fertnstert.2018.05.006.
- Aremu, Taiwo Opeyemi, et al. “Medication Adherence and Compliance: Recipe for Improving Patient Outcomes.” Pharmacy, vol. 10, no. 5, 28 Aug. 2022, www.ncbi.nlm.nih.gov/pmc/articles/PMC9498383/, https://doi.org/10.3390/pharmacy10050106.
- Zhang, Ge, and Daniel W. Nebert. “Personalized Medicine: Genetic Risk Prediction of Drug Response.” Pharmacology & Therapeutics, vol. 175, July 2017, pp. 75–90, https://doi.org/10.1016/j.pharmthera.2017.02.036.
- Stefanicka-Wojtas, Dorota, and Donata Kurpas. “Personalised Medicine—Implementation to the Healthcare System in Europe (Focus Group Discussions).” Journal of Personalized Medicine, vol. 13, no. 3, 21 Feb. 2023, p. 380, www.ncbi.nlm.nih.gov/pmc/articles/PMC10058568/, https://doi.org/10.3390/jpm13030380.
- Fuller, Joanne M., et al. “Why Do Patients Struggle with Their Medicines?—a Phenomenological Hermeneutical Study of How Patients Experience Medicines in Their Everyday Lives.” PLOS ONE, vol. 16, no. 8, 6 Aug. 2021, p. e0255478, www.ncbi.nlm.nih.gov/pmc/articles/PMC8345846/, https://doi.org/10.1371/journal.pone.0255478.
- Ingersoll, Karen S., and Jessye Cohen. “The Impact of Medication Regimen Factors on Adherence to Chronic Treatment: A Review of Literature.” Journal of Behavioral Medicine, vol. 31, no. 3, 1 June 2008, pp. 213–224, www.ncbi.nlm.nih.gov/pmc/articles/PMC2868342/, https://doi.org/10.1007/s10865-007-9147-y.
- Rohatgi, Karthik W., et al. “Medication Adherence and Characteristics of Patients Who Spend Less on Basic Needs to Afford Medications.” The Journal of the American Board of Family Medicine, vol. 34, no. 3, 1 May 2021, pp. 561–570, www.jabfm.org/content/34/3/561.abstract, https://doi.org/10.3122/jabfm.2021.03.200361.
- Geruso, Michael, et al. “Will Personalized Medicine Mean Higher Costs for Consumers?” Harvard Business Review, 1 Mar. 2018, hbr.org/2018/03/will-personalized-medicine-mean-higher-costs-for-consumers.
- Brown, Marie T., and Jennifer K. Bussell. “Medication Adherence: WHO Cares?” Mayo Clinic Proceedings, vol. 86, no. 4, Apr. 2011, pp. 304–314, www.ncbi.nlm.nih.gov/pmc/articles/PMC3068890/, https://doi.org/10.4065/mcp.2010.0575.
- Nieuwlaat, Robby, et al. “Interventions for Enhancing Medication Adherence.” Cochrane Database of Systematic Reviews, vol. 11, no. 11, 20 Nov. 2014, https://doi.org/10.1002/14651858.cd000011.pub4.