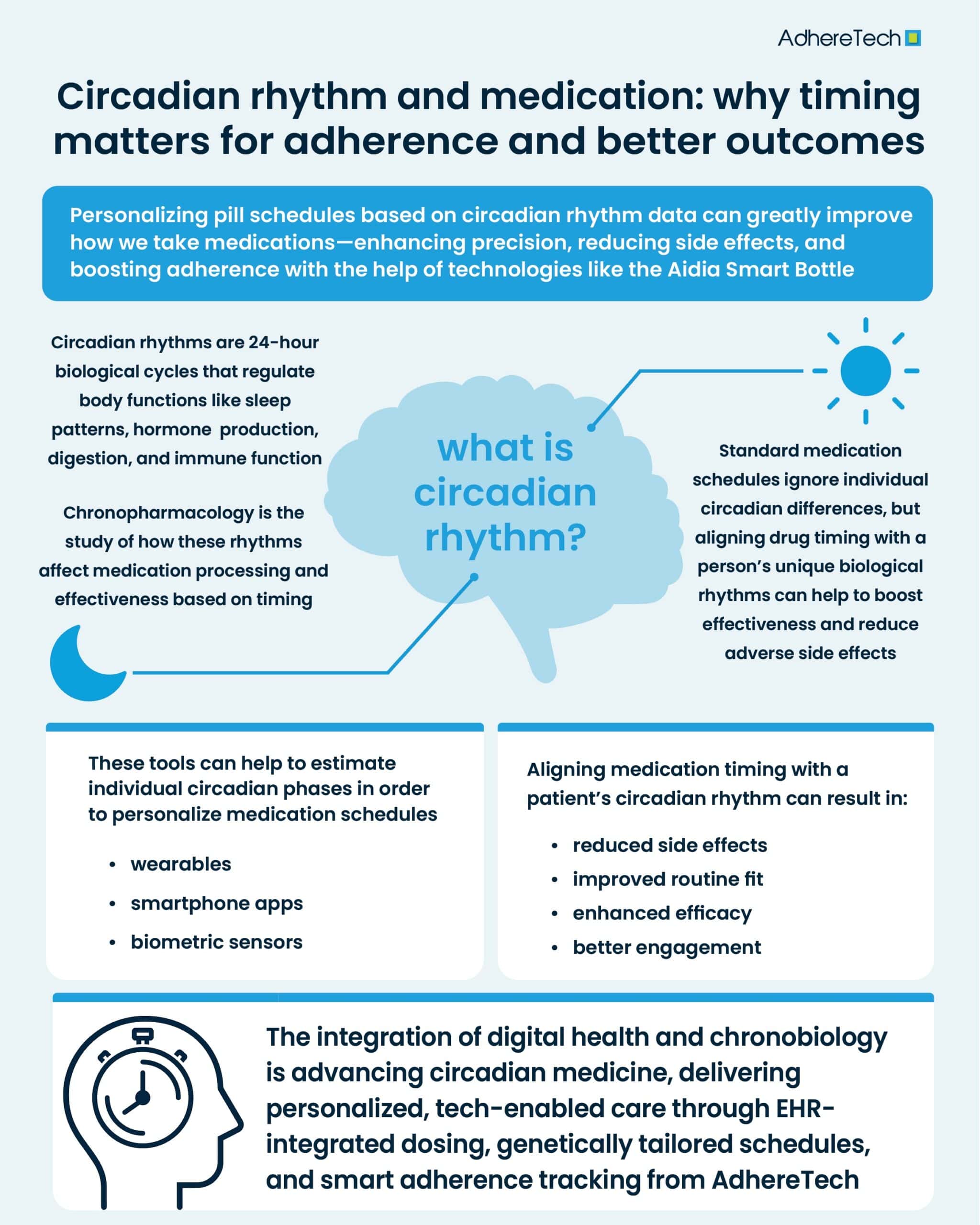
Personalizing pill schedules using circadian rhythm data could revolutionize how we take medications. As our understanding of the circadian system deepens, it’s clear that when we take medicine matters just as much as what we take. By embracing circadian rhythm data to personalize pill schedules, we unlock new levels of treatment precision and adherence support.
For patients and healthcare providers alike, this represents a win-win, with better outcomes, fewer side effects, and a more seamless approach to medication taking.
What Is Circadian Rhythm and Why Does It Matter?
Circadian rhythms are 24-hour biological cycles that regulate sleep-wake patterns, hormone production, digestion, and even immune function1. These internal clocks are influenced by external cues such as light and temperature, but they are also genetically regulated and highly individualized2.
When it comes to medication efficacy, timing can significantly affect how drugs are absorbed, distributed, metabolized, and excreted by the body3. This concept is known as chronopharmacology—the science of how the effects of drugs change according to the time of day3.
The Link Between Medication Timing and Effectiveness
Several studies have demonstrated that timing medication to align with circadian rhythms can enhance efficacy and reduce side effects4,5. For example, blood pressure medications taken at night can be more effective in reducing cardiovascular risk6, as blood pressure follows a diurnal rhythm—generally lowering at night (a phenomenon known as nocturnal dipping) and increasing in the morning7. Statins, used to lower cholesterol, work best when taken in the evening because the liver produces more cholesterol at night8. Asthma medications timed to the early morning can help mitigate the early-morning drop in lung function common in asthma patients9. These examples illustrate how synchronizing drug delivery with biological rhythms can lead to better health outcomes.
The Role of Personalization in Pill Scheduling
Generic medication schedules—“take one pill every 8 hours” or “once daily”—do not consider individual differences in circadian rhythm. People have different chronotypes, and these differences can influence the optimal time for medication intake. Personalizing medication dosing schedules based on an individual’s chronotype and biological rhythms can significantly improve a drug’s efficacy and safety10. This approach acknowledges that physiological processes such as hormone secretion, enzyme activity, and drug metabolism follow circadian patterns, which vary between individuals. Aligning drug administration with these rhythms—known as chronotherapy—has been shown to enhance therapeutic outcomes and minimize adverse effects11. For example, the use of chronotherapy when administering chemotherapy has been shown to increase tumor response and reduce toxicity12.
By leveraging data from wearables, smartphone apps, and biometric sensors, healthcare providers can now estimate individual circadian phases more accurately13. This makes it possible to personalize medication schedules so they are both biologically appropriate and easier for patients to follow. However, without robust, real-time adherence monitoring, whether patients adhere to this personalized schedule remains unknown, potentially limiting the prospective benefits.
Medication Adherence: The Hidden Crisis in Healthcare
One of the most overlooked factors influencing medication adherence is scheduling complexity and timing mismatches with the patient’s lifestyle or natural rhythms. Aligning medication timing with a patient’s circadian rhythm can reduce common barriers to adherence:
- Reduced Side Effects: Timing medications when the body is best equipped to process them can minimize adverse effects3.
- Improved Routine Fit: Medications that fit seamlessly into daily routines are more likely to be taken consistently14.
- Enhanced Efficacy: When patients experience quicker or more noticeable benefits, they are more motivated to stick with treatment1.
- Better Engagement: The use of personalized tools creates a sense of control and partnership in care, which has been linked to higher adherence16.
In short, personalization can enhance outcomes whilst simultaneously improving a patient’s experience with their medication.
The Future: Circadian Medicine and Digital Therapeutics
The convergence of digital health and chronobiology is paving the way for the new field of circadian medicine. In the future, we may see EHR-integrated systems that suggest optimal dosing times, pharmacogenomic tools that personalize schedules based on genetic markers, and even insurance incentives for adherence supported by smart tracking tools.
These developments could transform patient care by making it more individualized, effective, and sustainable.
References
- National Institute of General Medical Sciences. “Circadian Rhythms | National Institute of General Medical Sciences.” Nih.gov, 2017, nigms.nih.gov/education/fact-sheets/Pages/circadian-rhythms.
- Bass, Joseph, and Mitchell A. Lazar. “Circadian Time Signatures of Fitness and Disease.” Science (New York, N.Y.), vol. 354, no. 6315, 25 Nov. 2016, pp. 994–999, pubmed.ncbi.nlm.nih.gov/27885004/, https://doi.org/10.1126/science.aah4965. Accessed 13 Aug. 2021.
- Bicker, Joana, et al. “Timing in Drug Absorption and Disposition: The Past, Present, and Future of Chronopharmacokinetics.” British Journal of Pharmacology, vol. 177, no. 10, 20 Mar. 2020, pp. 2215–2239, https://doi.org/10.1111/bph.15017.
- Cezar-Ivan Colita, et al. “Optimizing Chronotherapy in Psychiatric Care: The Impact of Circadian Rhythms on Medication Timing and Efficacy.” Clocks & Sleep, vol. 6, no. 4, 5 Nov. 2024, pp. 635–655, www.mdpi.com/2624-5175/6/4/43, https://doi.org/10.3390/clockssleep6040043. Accessed 18 Nov. 2024.
- Walton, James C., et al. “Circadian Variation in Efficacy of Medications.” Clinical Pharmacology & Therapeutics, vol. 109, no. 6, 29 Nov. 2020, pp. 1457–1488, https://doi.org/10.1002/cpt.2073. Accessed 7 Mar. 2022.
- Lopez-Jimenez, Francisco. “Blood Pressure: Does It Have a Daily Pattern?” Mayo Clinic, 2019, www.mayoclinic.org/diseases-conditions/high-blood-pressure/expert-answers/blood-pressure/faq-20058115.
- X
- Wallace, A. “Taking Simvastatin in the Morning Compared with in the Evening: Randomised Controlled Trial.” BMJ, vol. 327, no. 7418, 4 Oct. 2003, pp. 788–788, www.ncbi.nlm.nih.gov/pmc/articles/PMC214096/, https://doi.org/10.1136/bmj.327.7418.788.
- Ukena, Dieter, et al. “Bronchial Asthma.” Deutsches Aerzteblatt Online, vol. 105, no. 21, 23 May 2008, www.ncbi.nlm.nih.gov/pmc/articles/PMC2696883/, https://doi.org/10.3238/arztebl.2008.0385.
- Smolensky, M. H., et al.Circadian rhythms and the optimization of cardiovascular drug therapy. Pharmacological Reviews, 71(2), 165–190 2019 https://doi.org/10.1124/pr.118.015305
- Ruben, M. D., et al. Dosing time matters. Science, 365(6453), 547–549 2019. https://doi.org/10.1126/science.aax7621
- Lévi, Francis, et al. “Implications of Circadian Clocks for the Rhythmic Delivery of Cancer Therapeutics.” Advanced Drug Delivery Reviews, vol. 59, no. 9-10, 31 Aug. 2007, pp. 1015–1035, pubmed.ncbi.nlm.nih.gov/17692427/, https://doi.org/10.1016/j.addr.2006.11.001.
- Shandhi, Md Mobashir Hasan, et al. “Taking the Time for Our Bodies: How Wearables Can Be Used to Assess Circadian Physiology.” Cell Reports Methods, vol. 1, no. 4, Aug. 2021, p. 100067, https://doi.org/10.1016/j.crmeth.2021.100067. Accessed 26 July 2022.
- Klinedinst, Tara C., et al. “The Roles of Busyness and Daily Routine in Medication Management Behaviors among Older Adults.” Journal of Applied Gerontology, vol. 41, no. 12, 11 Aug. 2022, p. 073346482211202, https://doi.org/10.1177/07334648221120246.
- Patcharin Khomkham, and Pootsanee Kaewmanee. “Patient Motivation: A Concept Analysis.” Belitung Nursing Journal, vol. 10, no. 5, 15 Oct. 2024, pp. 490–497, https://doi.org/10.33546/bnj.3529.
- Hein, Anna-Elisa, et al. “A Digital Innovation for the Personalized Management of Adherence: Analysis of Strengths, Weaknesses, Opportunities, and Threats.” Frontiers in Medical Technology, vol. 2, 14 Dec. 2020, https://doi.org/10.3389/fmedt.2020.604183.
- Lévi, Francis, et al. “Implications of Circadian Clocks for the Rhythmic Delivery of Cancer Therapeutics.” Advanced Drug Delivery Reviews, vol. 59, no. 9-10, 31 Aug. 2007, pp. 1015–1035, pubmed.ncbi.nlm.nih.gov/17692427/, https://doi.org/10.1016/j.addr.2006.11.001.