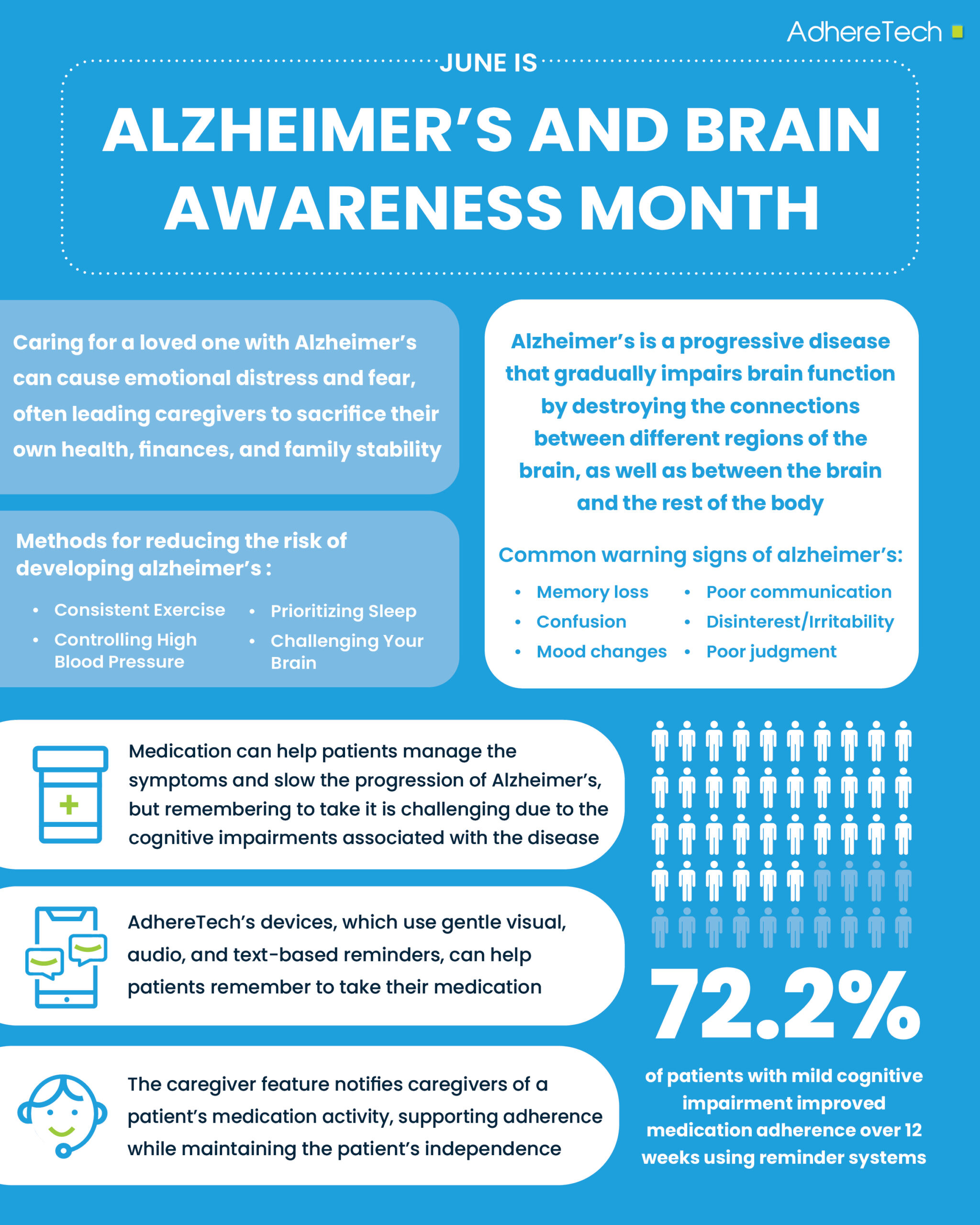
June marks Alzheimer’s and Brain Awareness Month, a month in which we come together to take action for ourselves and our loved ones in the fight to end Alzheimer’s.1 Alzheimer’s disease causes a progressive decline in brain functioning, with changes slowly destroying connective pathways between different regions of the brain, as well as the brain and body.2 The disease is typically defined by three stages. Firstly, are mild symptoms of cognitive impairment, such as memory loss and confusion due to the brain undergoing significant changes, including tissue loss, nerve death, and what are typically classified as hallmarks of the disease, abnormal build-ups of plaques and tangles.2 The second stage involves a continuation of negative brain alterations leading to more pronounced cognitive decline, with significant memory loss, poor spatial skills, and confusion.2 By the final stage, widespread cell death results in dramatic shrinkage of brain, particularly in the cortex, resulting in affected individuals losing their ability to communicate, recognize loved ones, and care independently for themselves.3
The progression of Alzheimer’s is extremely difficult for the individual experiencing it, but also for loved ones and caregivers. According to a Healthline poll4, the majority of caregivers sacrifice their own health, finances, and family dynamics for the sake of caring for a loved one with Alzheimer’s. Similarly, having a family history of Alzheimer’s does not determine, but increases one’s risk of developing the disease.5 Watching a family member deteriorate may spark fear and emotional distress, especially if one has concerns about facing the same diagnosis in the future.
Is there a Cure for Alzheimer’s Disease?
FDA-approved drugs can help patients manage the symptoms or slow the progression of Alzheimer’s disease.6 However, due to the cognitive impairments associated with the disease, remembering to take medications becomes increasingly challenging without reminder systems or caregiver support.7 Although no cure exists, for those with mild to moderate Alzheimer’s, existing medications can slow the disease’s progression7, which makes taking them as prescribed essential.
In one study, the implementation of reminder systems for patients with mild cognitive impairment resulted in 72.2% of patients showing improvement in taking their medications as prescribed over a 12 week duration.8 AdhereTech’s devices, including gentle visual, audio, and text-based reminders, can help support patients who may otherwise forget to take their medications. Additionally, the caregiver feature of these devices ensures caregivers receive notifications regarding a patient’s medication schedule and adherence, preserving patient autonomy whilst ensuring caregivers can provide additional support if necessary.
Most individuals with Alzheimer’s are over the age of 65+ and may face various age-related cognitive and physical impairments that can make opening medicine containers challenging.9, 10 For instance, research has shown that 14% of elderly adults were unable to open screw cap pill containers.11 Additional research indicates that up to 33% of 60+ year old patients use their containers incorrectly, with over 90% leaving the tops off or combining medications.12
AdhereTech was designed to address this issue with intuitive, easy-to-use devices, which 98% of older adults found accessible and effective. While the devices are easy for elderly patients to open, they are also 100% child-proof, balancing ease of access and safety. With a 98% effectiveness rating among older adults, indicating the ease of opening and using AdhereTech’s devices, the company’s products are designed to deliver accessible and easy-to-use adherence tools that meet the unique needs of aging populations. By tailoring its technology to the unique needs of aging populations, AdhereTech can play an essential role in promoting adherence and improving health outcomes for patients with Alzheimer’s disease.
What Can I Do to Reduce My Risk of Developing Alzheimer’s Disease?
Although no cure currently exists, the Alzheimer’s Association has released a list of healthy habits that can improve brain health, reducing one’s risk of developing Alzheimer’s disease.13
1. Challenge Your Brain → Challenging our brains by learning new skills or hobbies (such as painting, cooking, learning a new language, or instrument14) stimulates neuroplasticity, resulting in the brain strengthening existing neural pathways and creating new ones. This supports long-term brain health.13, 14
2. Get Your Workout In → Exercise can increase cerebral blood flow, increase the volume of mitochondria and the hippocampus, as well as improve neurogenesis, all of which can help to improve cognitive functioning.15
a) People who walked an estimated 5 miles per day, were 51% less likely to develop dementia compared to people who barely walked in a day.16
b) Walking just two miles per day has been shown to reduce the risk of developing dementia by 25%.16
3. Control and Reduce High Blood Pressure → High blood pressure can damage small blood vessels in the brain, resulting in reduced blood flow and oxygen delivery to brain cells. This can negatively impact brain areas responsible for thinking and memory.17
a) Adherence to a healthy diet, regular exercise, and (if needed) blood pressure medications can help lower blood pressure and preserve brain health.18
4. Manage Diabetes → For those with type 2 diabetes, poorly controlled blood pressure can lead to the build-up of amyloid (plaques) and tau (tangles) proteins in the brain, hallmarks of Alzheimer’s disease.19
a) Adherence to anti-diabetic medications, a healthy diet, a workout regimen, and weight management can help regulate blood pressure and brain health.20, 21
5. Prioritize Sleep → During the day, our brains produce beta-amyloid (a protein believed to be a hallmark of Alzheimer’s disease, commonly known as “plaques”), without adequate sleep our brain cells and connections cannot shrink allowing for beta-amyloid to be flushed away.22 This can lead to their accumulation, increasing the risk of cognitive decline.22
a) One study found that for those aged 50-70, sleeping 6 hours, as opposed to the recommended 7 hours, increased their risk of developing dementia by 30%.22
What Can I Do If I Suspect My Loved One Has Dementia?
The symptoms of Alzheimer’s disease vary from person to person, but they are most commonly defined by a gradual onset.23
1. Look for the warning signs24
a) Cognition-Related: Memory loss, confusion (particularly about time or place), difficulty with written and verbal communication, trouble with planning or thinking ahead, trouble with familiar tasks, poor judgement24
b) Personality-Related: Lack of interest, mood or personality changes (particularly increased irritability)24
***If these symptoms have been developing over time, they’re more likely to be dementia-related.***24
2) Talk with Close Family Members or Friends
a) Ask friends and family if they’ve noticed any changes in your loved one in a confidential and respectful manner.24
3. Talk to Your Loved One
a) Some individuals with early dementia may be aware of their memory difficulties, and may be relieved to be asked about it, while others may become defensive.24 When talking with your loved ones, be thoughtful and respectful.24
i) Use “I,” instead of “you” statements.24
ii) Use the term “memory problems” instead of Alzheimer’s.24
4. Try to Persuade Your Loved One to See a Healthcare Provider24
a) If you and others notice these warning signs, seeing a GP is recommended.23
i) Cognitive decline is not always Alzheimer’s… normal pressure hydrocephalus or a vitamin B12 deficiency can cause memory issues; both still require proper treatment.24
b) My loved one does not want to speak with a healthcare provider, what can I do?
i) Try reminding them they need their annual check-up.24
ii) Ask their healthcare provider to call and ask about scheduling an appointment.24
iii) Ask other family members to step in, for support.24
5. While no cure for Alzheimer’s exists, early diagnosis is important because…
a) Treatments are often most effective when started early in the disease process.25
b) It allows for participation in clinical trials to improve health outcomes and research.25
c) It allows the diagnosed individual time to make informed legal, financial, and care decisions.21
While the hunt for a cure for Alzheimer’s continues, numerous advances in the past decade prove promising. Numerous medicines, such as Lecanemab and Donanemab, have been approved by the FDA for reducing the symptoms of early Alzheimer’s disease.6 Furthermore, as of May 16th, 2025, the FDA cleared the first blood test to help in early detection of amyloid plaques in those exhibiting symptoms of Alzheimer’s disease.26 Each of these milestones brings us closer to a future where early diagnosis, treatment, and improved quality of life are not merely possibilities, but expectations in the diagnosis and treatment of Alzheimer’s disease.
References
1 Alzheimer’s Association. (2024). June is Alzheimer’s & Brain Awareness Month. https://www.alz.org/abam/overview.asp
2 UCLA Health. (2018, July 5). Ask the doctors: What is the cause of death in Alzheimer’s disease? https://www.uclahealth.org/news/article/ask-the-doctors-what-is-the-cause-of-death-in-alzheimers-disease
3 Alzheimer’s Association. (2024). Inside the brain: What is Alzheimer’s? https://www.alz.org/abam/overview.asp
4 Koskie, B., & Akers, W. (2024). Dealing with Alzheimer’s and its impact on family. Healthline. https://www.healthline.com/health/state-of-alzheimers
5 Harvard Health Publishing. (2019, Jan 28). Alzheimer’s in the family. Harvard Medical School. https://www.health.harvard.edu/mind-and-mood/alzheimers-in-the-family#:~:text=Family%20history%20by%20the%20numbers,absolute%20change%20is%20relatively%20small.
6 National Institute on Aging. (n.d.). How is Alzheimer’s disease treated? U.S. Department of Health and Human Services. https://www.nia.nih.gov/health/alzheimers-treatment/how-alzheimers-disease-treated
7 Arlt, S., Lindner, R., Rösler, A., & von Renteln-Kruse, W. (2008). Adherence to medication in patients with dementia: predictors and strategies for improvement. Drugs & aging, 25(12), 1033–1047. https://doi.org/10.2165/0002512-200825120-00005
8 Kamimura, T., Ishiwata, R., & Inoue, T. (2012). Medication reminder device for the elderly patients with mild cognitive impairment. American Journal of Alzheimer’s Disease & Other Dementias®, 27(4), 238-242.
9 Isik A. T. (2010). Late onset Alzheimer’s disease in older people. Clinical interventions in aging, 5, 307–311. https://doi.org/10.2147/CIA.S11718
10 Beckman, A., Bernsten, C., Parker, M. G., Thorslund, M., & Fastbom, J. (2005). The difficulty of opening medicine containers in old age: a population-based study. Pharmacy world & science : PWS, 27(5), 393–398. https://doi.org/10.1007/s11096-005-7903-z
11 Beckman, A. G., Parker, M. G., & Thorslund, M. (2005). Can elderly people take their medicine?. Patient education and counseling, 59(2), 186-191.
12 Jahnigen, D. W. (1988). Problems with pill packaging. Journal of the American Geriatrics Society, 36(3), 279-280.
13 Alzheimer’s Association. (n.d.). 10 healthy habits for your brain. https://www.alz.org/help-support/brain_health/10-healthy-habits-for-your-brain
14 Fisher, J. (2025, April 2). Tips to leverage neuroplasticity to maintain cognitive fitness as you age. Harvard Health Publishing. https://www.health.harvard.edu/mind-and-mood/tips-to-leverage-neuroplasticity-to-maintain-cognitive-fitness-as-you-age
15 Pahlavani, H. A. (2023). Exercise therapy to prevent and treat Alzheimer’s disease. Frontiers in Aging Neuroscience, 15, 1243869.
16 Godman, H. (2022). Walking linked to lower dementia risk. Harvard Medical School. https://www.health.harvard.edu/mind-and-mood/walking-linked-to-lower-dementia-risk
17 Johns Hopkins Medicine. (n.d.). Blood pressure and Alzheimer’s risk: What’s the connection? https://www.hopkinsmedicine.org/health/conditions-and-diseases/alzheimers-disease/blood-pressure-and-alzheimers-risk-whats-the-connection
18 National Heart, Lung, and Blood Institute. (2024). High blood pressure treatment. National Institute of Health. https://www.nhlbi.nih.gov/health/high-blood-pressure/treatment
19 Alzheimer’s Society. (2024). Diabetes and the risk of dementia. https://www.alzheimers.org.uk/about-dementia/managing-the-risk-of-dementia/reduce-your-risk-of-dementia/diabetes
20 Sahoo, J., Mohanty, S., Kundu, A., & Epari, V. (2022). Medication Adherence Among Patients of Type II Diabetes Mellitus and Its Associated Risk Factors: A Cross-Sectional Study in a Tertiary Care Hospital of Eastern India. Cureus, 14(12), e33074. https://doi.org/10.7759/cureus.33074
21 Mayo Clinic. (n.d.). Type 2 diabetes. https://www.mayoclinic.org/diseases-conditions/type-2-diabetes/diagnosis-treatment/drc-20351199
22 Budson, A. (2021). Sleep well – and reduce your risk of dementia and death. Harvard Medical School. https://www.health.harvard.edu/blog/sleep-well-and-reduce-your-risk-of-dementia-and-death-2021050322508
23 National Institute of Aging. (2022). What are the signs of Alzheimer’s disease? https://www.nia.nih.gov/health/alzheimers-symptoms-and-diagnosis/what-are-signs-alzheimers-disease
24 Heerema, E. (2023). If you think a loved one has dementia. Verywell Health. https://www.verywellhealth.com/what-to-do-if-a-loved-one-may-have-alzheimers-98048
25 Alzheimer Society. (n.d.). The 10 benefits of early diagnosis. https://alzheimer.ca/en/about-dementia/do-i-have-dementia/how-get-tested-dementia-tips-individuals-families-friends/10
26 U.S. Food and Drug Administration. (2025, May 16). FDA clears first blood test used in diagnosing Alzheimer’s disease. https://www.fda.gov/news-events/press-announcements/fda-clears-first-blood-test-used-diagnosing-alzheimers-disease