Definition: Glaucoma is a group of diseases that can cause significant damage to the optic nerve, the part of the eye that sends electrical impulses for sight to the brain.1
How Does Glaucoma Occur?
Glaucoma develops when damage to the optic nerve occurs, typically in relation to increased pressure in the eye.2 Raised eye pressure is oftentimes a result of a buildup of fluid that moves throughout the inside of the eye, called aqueous humor.2 Under optimal conditions, aqueous humor drains through the trabecular meshwork, a tissue where the iris and cornea meet.2 However, when the produces too much fluid or the drainage system fails, this can result in increases in eye pressure.2
The following elaborates upon how each type of glaucoma may occur:
- Open-angle glaucoma
- Acute angle-closure glaucoma
- Normal-tension glaucoma
- For normal tension glaucoma, it remains unknown why the optic nerve becomes damaged when the eye pressure remains healthy.2 It is suspected that the optic nerve may be sensitive or experience less blood flow, which may be caused by the buildup of fatty deposits in the arteries or other conditions that damage circulation.2
- Glaucoma in children
- Pigmentary glaucoma
- In pigmentary glaucoma, small pigment granules fall off from the iris, slowing or blocking fluid drainage from the eye.2 Activities as simple as jogging may stir up these pigment granules, leading to deposits on the tissue located where the iris and cornea meet.2 Over time, these granule deposits cause an increase in pressure.2
Symptoms of Glaucoma:
The symptoms of glaucoma are dependent on the type and stage of the condition. However, it is important to note that oftentimes, there are no initial symptoms of glaucoma.1, 2
- Open-angle glaucoma
- The symptoms of open-angle glaucoma are often minimal to none when the disease begins, with individuals experiencing no eye pain or visual impairments.1, 2
- As the disease progresses, individuals may begin to experience side vision failure1, 2 Side vision failure entails an individual being able to see objects straight ahead of them clearly, but struggling to see objects within the side of their vision.1, 2
- As the disease progresses into later stages, without proper treatment, people living with glaucoma may lose their ability to see objects straight ahead as well.1, 2
- Acute angle-closure glaucoma
- Symptoms include bad headaches, severe eye pain, nausea and/or vomiting, blurred vision, halos or colored rings around lights, and eye redness.2
- Normal-tension glaucoma
- The symptoms of open-angle glaucoma are often minimal to none when the disease begins, with individuals experiencing no eye pain or visual impairments.1, 2
- As the disease progresses, individuals may begin to experience partial blind spots in their side vision or side vision failure.1, 2 Side vision failure entails an individual being able to see objects straight ahead of them clearly, but struggling to see objects within the side of their vision.1, 2
- As the disease progresses into later stages, without proper treatment, people living with glaucoma may lose their ability to see objects straight ahead as well.1, 2
- Glaucoma in children
- Pigmentary glaucoma
- Symptoms include blurred vision with exercise, seeing halos around lights, and gradual loss of side vision.2
Individuals with Genetic Predisposition or Risk Factors
Glaucoma has the ability to cause visual damage and impairments before any noticeable symptoms occur, making it critical to be aware of risk factors for glaucoma.2 Risks factors include …
- High internal eye pressure (intraocular pressure).2
- Age, over 55.2
- This is likely due to aging increasing the optic nerve’s vulnerability, making the optic nerve more susceptible to various challenges, such as increased eye pressure due to weakening of the pathway through which the aqueous humor discharges from the eye.4
- Black, Asian, or Hispanic heritage.2
- Certain forms of glaucoma occur more frequently or more aggressively in these marginalized patient populations.5 For instance, primary open angle glaucoma (POAG) is diagnosed 10 years earlier and shows more rapid progression among African American patients.5 There is also a higher confirmed prevalence of glaucoma among African Americans outside of the United States, such as in Barbados, the West Indies, and East Africa.5 Notably, in LatinX populations, multiple genetic variants have been associated with increased risk of developing glaucoma, such as vertical cup-disc ratio and central corneal thickness.5
- Certain medical conditions, such as diabetes, migraine, high blood pressure, and sickle cell anemia.2
- Corneas that are thin in the center.2
- Extreme nearsightedness or farsightedness.2
- Eye injury or certain types of eye surgery.2
- Taking corticosteroid medicines, especially eye drops, for extended durations of time.2
- Narrow drainage angles that can put an individual at an increased risk of angle-closure glaucoma.2
How is Glaucoma Detected
Due to the most common forms of glaucoma often lacking initial symptoms, testing is vital.1 A comprehensive dilated eye exam, in which drops are placed into the eyes to enlarge the pupils, allows professionals to check the inside of the eye for signs of optic nerve damage.1 Screening for eye pressure alone is not enough to detect glaucoma, making a comprehensive dilated eye examination imperative.1
Treatment and the Challenges Associated with Medication Adherence
Currently, there is no cure for glaucoma; however, treatment can help to control eye pressure and prevent further damage to the optic nerve.1 The first line of treatment typically entails medication, progressing to laser or traditional surgery if eye pressure cannot be controlled with medication.1
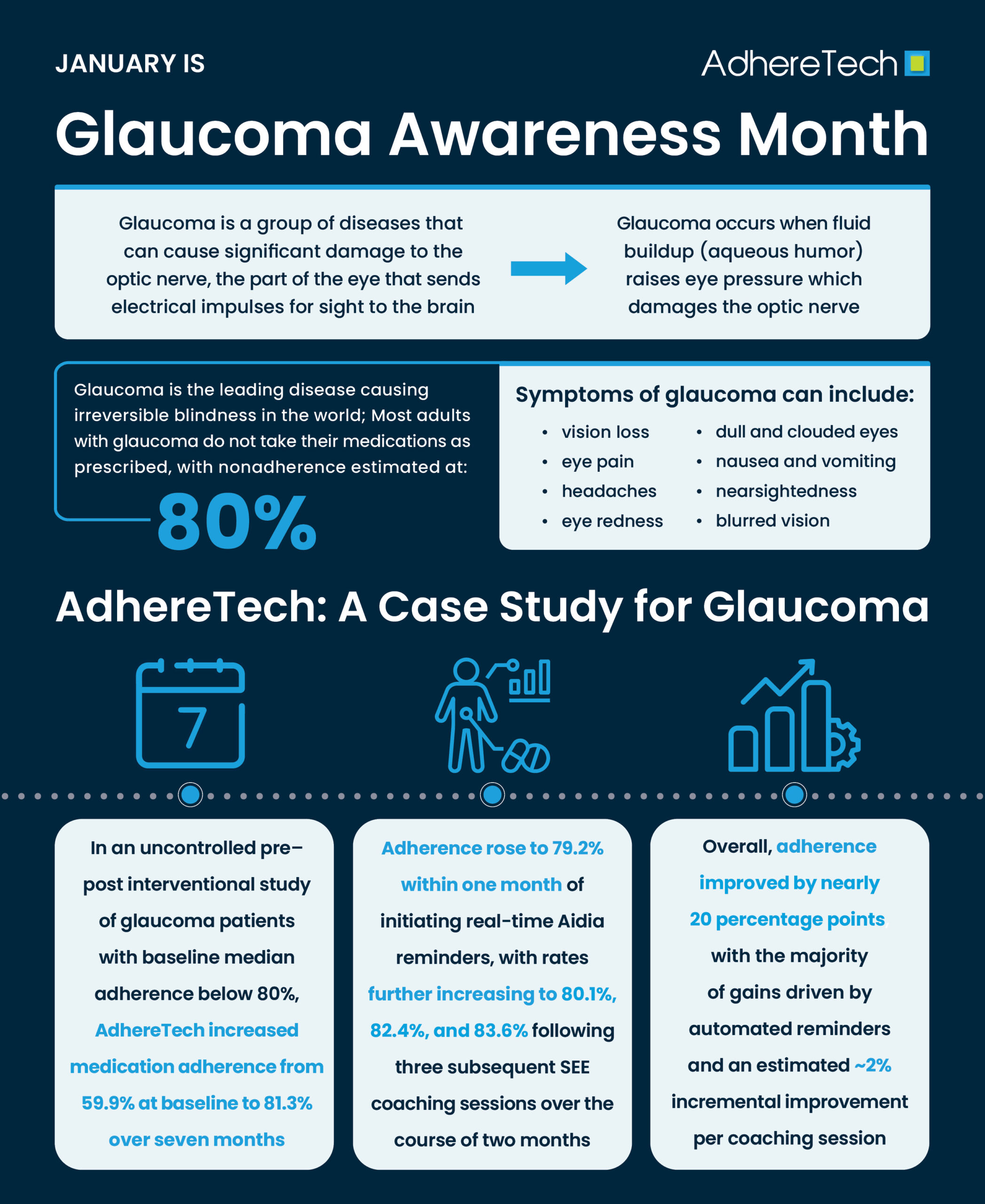
Despite the widespread availability of effective treatment for glaucoma, glaucoma is the leading disease causing irreversible blindness in the world, disproportionately affecting marginalized patient populations.6 This may be due to an estimated 80% of adults with glaucoma not taking their medications as prescribed, with poorer medication adherence associated with greater losses in vision from glaucoma.6 Logistical regression analysis of 185 questionnaires administered to patients living with glaucoma found the following barriers were associated with higher rates of non-adherence …
- Forgetfulness, OR = 5.6 [95% CI 2.6–12.1, p= < 0.0001].7
- Decreased self-efficacy, OR = 4.7 [95% CI 2.2–9.7, p= < 0.0001].7
- Difficulties with the medication schedule, OR = 2.9 [1.4–6.0, p= 0.006].7
- Difficulty instilling drops, OR = 2.3 [95% CI 1.1–4.9, p= 0.03].7
Additional reported barriers to adherence for those living with glaucoma include …
- Medication costs, particularly for those of low socioeconomic status.6
- Psycho-social issues, including skepticism that an asymptomatic condition can result in permanent blindness and/or a lack of trust in healthcare providers.6
AdhereTech
Research consistently highlights that medication adherence presents a large barrier to effectively treating glaucoma.6, 7 Even patients who are prescribed medications that can prevent further vision loss often struggle to remain adherent to their prescribed regimens. Forgetfulness, complex medication schedules, difficulty with eye drop administration, and psychosocial factors all contribute to poor adherence outcomes, which can lead to irreversible vision damage.6, 7
AdhereTech is designed to overcome these barriers through its smart, patient-centered Aidia system.
Reminders and Alerts for Timely Dosing
AdhereTech’s smart devices arrive pre-programmed with each patient’s individualized glaucoma medication schedule, ensuring that reminders are tailored to their dosing needs. The system provides real-time, customizable alerts to help patients remember each dose and reduce the cognitive burden associated with complex medication regimens.
The reminder escalation sequence is designed to maximize adherence without being intrusive: a gentle glow signals the upcoming dosing window, followed by a chime every 15 minutes during the window if the dose is not yet taken. If a dose is still missed, an SMS notification is sent to the patient, prompting them to either take the medication or provide an explanation for their missed or delayed dose. This continuous feedback loop supports patients in staying on schedule, reinforces adherence habits, and allows healthcare providers to monitor missed doses in real time – critical for preventing the silent progression of glaucoma and protecting vision.
Simplifying complex Medication Regimens
AdhereTech’s devices arrive pre-programmed with each patient’s individualized glaucoma medication schedule, supporting consistent use of a single prescribed eye drop. By providing a consistent escalatory reminder sequence, Aidia helps patients stay on track without confusion, ensuring that each dose is taken at the correct time and in the proper amount.
Using an electronic magnetic field, AdhereTech’s smart pill bottle can detect if too much or too little medication is removed from the bottle, alerting patients’ healthcare professionals of dosing errors in real time. This feature ensures accurate administration, reinforcing safe and effective use.
The system also reduces the mental burden of remembering daily dosing, allowing patients to incorporate their eye care into their routines seamlessly. Real-time monitoring of both timing and dose enables healthcare providers to intervene promptly if adherence or dosing issues arise. This targeted support can help to ensure eye pressure remains controlled, preventing progressive optic nerve damage that could lead to vision loss.
Data-Driven Support for Healthcare Providers
AdhereTech automatically logs each dose taken, offering real-time adherence data to healthcare professionals. This allows clinicians to track patterns of missed doses, identify potential barriers, and intervene proactively.
For glaucoma patients, whose disease often progresses silently, this continuous feedback is critical. Providers can review adherence trends, adjust treatment plans, and deliver targeted education or support before irreversible optic nerve damage occurs. This data-driven approach fosters a therapeutic alliance among patients and healthcare professionals, preserving patient autonomy while protecting their health.
Assistance with Eye Drop Administration
Correctly administering eye drops can be challenging, especially for older adults or patients with limited dexterity. AdhereTech addresses this barrier by providing timely, actionable reminders and allowing patients to report reasons for non-adherence, such as difficulty with drop administration. Customizable text reminders can offer step-by-step guidance or be escalated to healthcare professionals if additional support is needed.
The reminder sequence, including a gentle glow, chimes every 15 minutes during the dosing window, and SMS alerts for missed doses, encourage patients to complete each dose properly. Over time, this continuous reinforcement builds self-efficacy, helping patients develop reliable habits and master the correct technique. By supporting proper administration, Aidia ensures medications are effective, directly reducing the risk of progressive glaucoma and vision loss.
Accessibility Across Populations
Glaucoma disproportionately affects older adults and marginalized populations, who may be at an increased risk of facing barriers such as limited technology access or literacy, language differences, or low health literacy. AdhereTech devices are designed to be inclusive: they operate without Wi-Fi or smartphones via cellular data, offer reminders in the patient’s first language, and communicate in clear, health-literate language. Furthermore, the device’s combination of universal reminders, including a gentle glow and chime, helps to ensure that even patients with visual impairments who may struggle to read SMS messages receive understandable reminders. The ability for patients to receive calls, instead of SMS calls, when a missed dose occurs helps to further ensure that all patients are able to receive the support they deserve along their medication adherence journeys.
Patients receive reminders and feedback in ways that fit their lifestyle and technology comfort level, ensuring equitable access to adherence support. By removing these barriers, Aidia helps all patients, including those from underserved communities, maintain consistent eye drop use, protecting vision and reducing disparities in glaucoma outcomes.
AdhereTech: A Case Study for Glaucoma
AdhereTech’s ability to effectively support patients living with glaucoma has been validated via an uncontrolled interventional study with pre-post design.6 Prior to enrollment, all patients had a median adherence rate of less than 80%, indicating they were classified as nonadherent to their prescribed treatment.6 Patients received AdhereTech’s smart pill bottle, personalized coaching sessions, and 5 phone calls for in-between counseling session support. Adherence improved from 59.9% at baseline to 81.3% (p < 0.0001) at the conclusion of the 7 month program.6
Notably, baseline adherence was estimated at 59.9%, but improved to 79.2% (SD = 17.6%, p < 0.0001) just one month after patients began receiving medication reminders through AdhereTech’s Aidia system.6 Subsequent SEE coaching sessions further reinforced adherence, with rates increasing to 80.1% (SD = 20.6%; p = 0.58), 82.4% (SD = 18.6%; p = 0.049), and 83.6% (SD = 17.5%; p = 0.020) during the two-month periods following each of the three sessions.6 While each coaching session contributed an estimated 2% improvement, the majority of the nearly 20% overall increase in adherence was achieved through the real-time reminders and support provided by AdhereTech, underscoring the system’s substantial ability to enhance medication adherence.
Conclusion
Due to glaucoma having the ability to cause gradual vision loss without noticeable symptoms, awareness, early detection, and consistent treatment are essential to protecting optic nerve health and preserving vision. However, even though effective medications are available, adherence remains an overarching challenge in proper treatment.
AdhereTech addresses these challenges through its smart, patient-centered Aidia system. By providing real-time reminders, dose monitoring, and data-driven support for healthcare providers, AdhereTech empowers patients to take their glaucoma medications consistently and correctly. The nearly 20% improvement in adherence observed in a clinical study demonstrates the system’s potential to transform real-world outcomes for patients living with glaucoma.6 With the right tools and consistent habits, vision loss from glaucoma can be slowed or prevented, preserving quality of life for years to come.
References
1 National Eye Institute. (National Eye Institute. (2019). Facts about glaucoma (Fact sheet). National Institutes of Health. https://www.nei.nih.gov/sites/default/files/2019-06/Facts-about-glaucoma.pdf National Eye Institute
2 Mayo Clinic Staff. (2024, November 5). Glaucoma: Symptoms and causes. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/glaucoma/symptoms-causes/syc-20372839
3 Guedes, G., Tsai, J. C., & Loewen, N. A. (2011). Glaucoma and aging. Current aging science, 4(2), 110–117. https://doi.org/10.2174/1874609811104020110
4 Ou, Y. (2021, August 23). Age and glaucoma. BrightFocus Foundation. https://www.brightfocus.org/resource/age-and-glaucoma/
5 Siegfried, C. J., & Shui, Y. B. (2022). Racial Disparities in Glaucoma: From Epidemiology to Pathophysiology. Missouri medicine, 119(1), 49–54.
6 Newman-Casey, P. A., Niziol, L. M., Lee, P. P., Musch, D. C., Resnicow, K., & Heisler, M. (2020). The impact of the support, educate, empower personalized glaucoma coaching pilot study on glaucoma medication adherence. Ophthalmology Glaucoma, 3(4), 228-237.
7 Newman-Casey, P. A., Robin, A. L., Blachley, T., Farris, K., Heisler, M., Resnicow, K., & Lee, P. P. (2015). The Most Common Barriers to Glaucoma Medication Adherence: A Cross-Sectional Survey. Ophthalmology, 122(7), 1308–1316. https://doi.org/10.1016/j.ophtha.2015.03.026