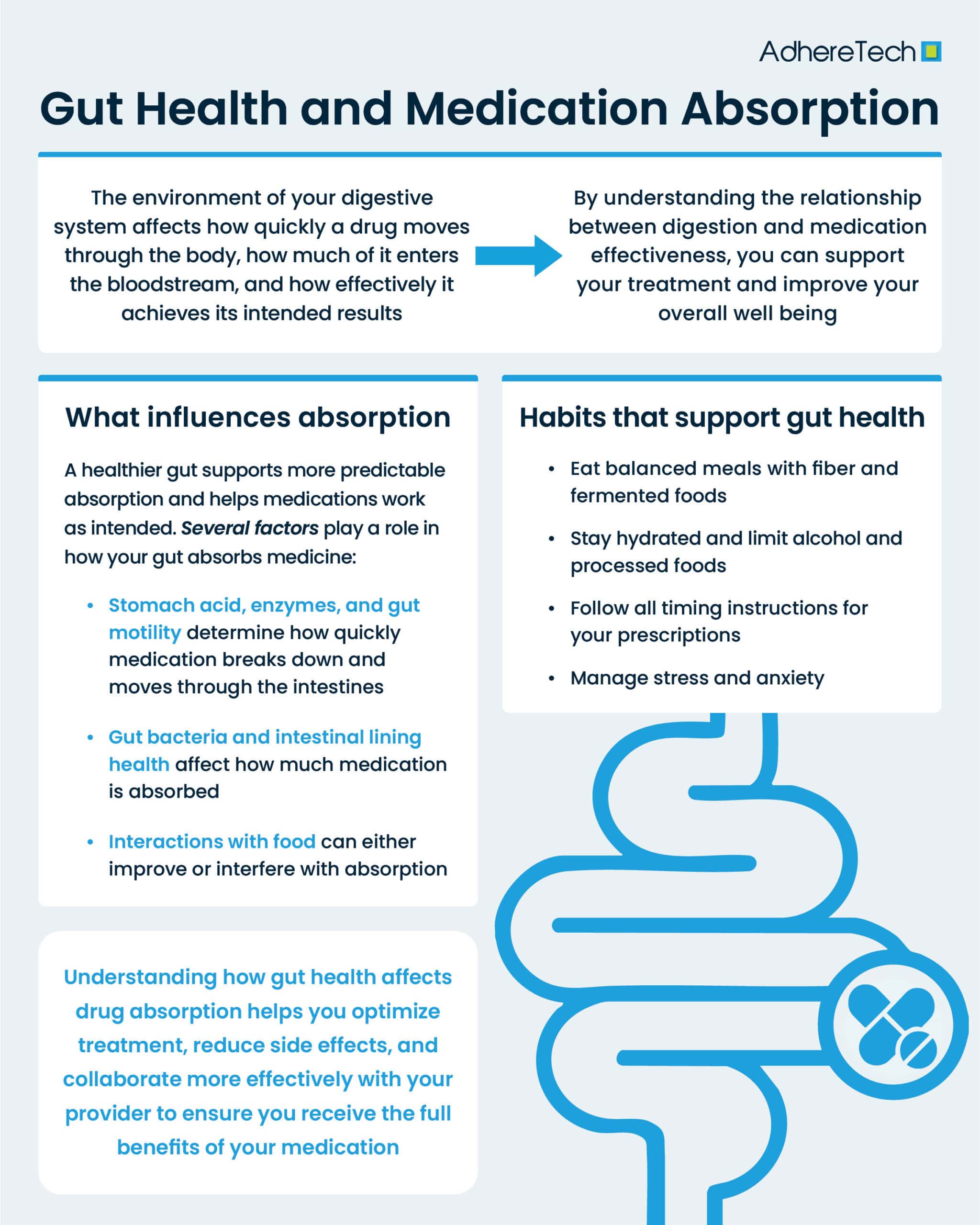
Your gut does far more than break down food—it plays a vital role in nutrient absorption, immune function, and even mood regulation via the brain-gut connection.1 Yet one important aspect of gut health often goes unnoticed: its influence on how well medications work.2 Despite the fact that many medications rely on the gut as their primary pathway into the body, this connection is often underestimated when compared other domains of gut health. The environment of your digestive system, including stomach acidity, enzyme activity (how well a person’s body breaks things down in the gut), microbiome balance (the mix of good and bad bacteria within the gut), and overall gut motility (the speed at which food and medicine moves through the gastrointestinal system), can affect how quickly a drug moves through the body, how much of it enters the bloodstream, and how effectively it is at achieving its intended results.2
When the gut is inflamed, imbalanced, or simply not functioning at its optimal level, medications may be absorbed too quickly, too slowly, or not fully at all.2 Conversely, maintaining a healthy gut can support more predictable and efficient absorption.2 If you take prescription medications or supplements, understanding the connection between gut health and drug absorption can help you optimize your treatment, minimize side effects, and work more effectively with your healthcare provider to ensure you receive your medication’s full benefits, while reducing your risk of unintended side effects and/or additional complications.3
Why Gut Health Matters for Medication Absorption
After you swallow a pill, capsule, or liquid, it passes through the stomach and intestines before being absorbed into the bloodstream, where it can then travel to the rest of the body.4 Throughout this journey, the medication must dissolve properly, survive the environment of the stomach, and pass through the intestinal wall, all steps that require a well-functioning digestive system.5 Because this entire process depends on healthy digestion, anything that affects how your gut functions also has the potential to influence how well a medication works.2
Several factors play a role in how well your gut absorbs medicine:4
- Stomach acid levels
- Digestive enzyme activity
- Gut motility or how quickly food and medicine move through the system
- The balance of gut bacteria
- The health of the intestinal lining
- Interactions with food and other substances
When any of these elements are disrupted, medication absorption may change.2,4 This does not inherently suggest that the medication itself is ineffective or problematic. Instead, the digestive environment may need attention.4
The Role of Stomach Acid
Stomach acid not only breaks down food but also helps prepare many medications for absorption.6 Some drugs rely on the stomach’s naturally acidic environment to dissolve properly, while others need protection from excess acid and are formulated with special coatings to prevent them from breaking down too quickly.6
To appreciate why stomach acidity matters, it helps to look at the pH scale—a measure of how acidic or basic a substance is. The scale runs from 0 to 14, with lower numbers indicating higher acidity. While the small intestine has a relatively mild pH of about 6.6, the stomach is extremely acidic, typically around pH 1.7
When stomach acid levels are lower than normal, certain medications may dissolve more slowly or be absorbed less effectively. In contrast, high stomach acid can cause other drugs to break down too quickly.6 Conditions like acid reflux, gastritis, or long-term use of acid-reducing medications can all influence your stomach’s acidity,8 and in turn, medication absorption.
If you take medications that depend on specific acid conditions to work effectively, such as those with enteric coatings, your healthcare provider may give timing instructions, such as taking the medication before meals, with meals, or on an empty stomach, to help ensure optimal absorption.9 These guidelines can help to ensure that the drug reaches the correct part of the digestive tract at the intended time, ensuring maximum efficacy.
Gut Motility and Transit Time
Gut motility refers to the speed at which material moves through your digestive system.10 When motility is too fast, medications may travel through the gut before they have time to become fully absorbed, reducing their efficacy.11 When it’s too slow, medications can linger longer than intended, potentially altering their dose release timing, effectiveness, or even causing stronger, unpleasant side effects.11
A variety of factors can influence gut motility, including diarrhea, constipation, irritable bowel syndrome, and infections.11 Even stress and anxiety can speed up or slow down digestion by affecting the gut–brain connection.12 When your digestive rhythm is disrupted, it can change the speed at which medications move through the system—and ultimately how well they work.11
The Gut Microbiome
Your gut is home to trillions of bacteria that play a crucial role in breaking down food, supporting immune function, and maintaining the integrity of the intestinal lining.13 These microorganisms can also interact directly with medications: some bacteria help activate certain drugs, while others may break them down too early or compete with them for absorption, potentially altering their effectiveness.13
Factors such as antibiotics, dietary changes, illness, and stress can shift the balance of gut bacteria, sometimes disrupting the delicate ecosystem of your microbiome.13 When this balance is disturbed, it can affect the efficacy and toxicity of drugs, which can vary significantly from person to person due to the high variability of the gut microbiota.14 Maintaining a healthy, diverse gut microbiome can support stable, predictable digestion, which in turn helps medications work more consistently and reliably.14
The Intestinal Lining
Your small intestine is where most oral medications are absorbed.15 Its lining functions as a selective gate, allowing certain substances to pass into the bloodstream while keeping others out. When this lining becomes irritated, inflamed, or damaged, medication absorption can be reduced, potentially affecting how well treatments work.15
Several factors can impact the health of the intestinal lining, including conditions such as celiac disease, inflammatory bowel disease, chronic infections, and prolonged stress.16 Even frequent use of certain over-the-counter pain relievers can irritate the gut.1 When the intestinal lining is not functioning optimally, medications may enter the bloodstream less efficiently, which can alter their effectiveness and the timing of their action.16 Maintaining gut health is therefore an important factor in ensuring medications perform as intended.3
Food and Medication Interactions
What you eat can significantly influence how well your gut absorbs medications.2 Certain foods can slow absorption, while others may speed it up.2 Specific nutrients can either block or enhance the uptake of medications, affecting how effectively they work.1
For example:
- High-fiber meals may delay absorption for some medications due to fiber moving throughout the digestive tract without being digested or absorbed. Excess amounts of fiber in the intestine at the same time as a medication may result in the medication being moved with the fiber, resulting in excess excretion as opposed to absorption.17
- Grapefruit contains compounds that inhibit enzymes responsible for metabolizing certain medications, which can lead to elevated drug levels in the bloodstream and potentially intensify their effects.18
- Calcium-rich foods can reduce absorption of some antibiotics due to calcium binding to antibiotics, subsequently reducing their absorption and effectiveness.19
- High-fat foods can affect how certain medications are absorbed. When some drugs are taken with high-fat meals, they may produce higher blood levels, increasing the risk of toxicity or unwanted side effects, while others may become less effective.20
Timing also plays a key role. Some medications are most effective when taken on an empty stomach, while others require food to prevent irritation or improve absorption.21 Following the instructions provided with your medication—and discussing any questions or concerns regarding your prescribed regimen(s) with your healthcare provider—can help ensure you get the best results for your specific situation.
Hydration and Digestive Function
Water plays a crucial role in digestion by helping break down food, move medications through the digestive tract, and support the integrity of the intestinal lining.22 Dehydration can slow digestion, lead to constipation, or increase stomach acidity—all of which can affect how quickly and efficiently medications are absorbed.22
Maintaining consistent hydration helps create a balanced digestive environment, supporting smooth digestion and allowing medications to work as intended.23
When to Talk to Your Healthcare Provider
You should reach out to your provider if:
- Your medication is not controlling your symptoms as indended.
- A medication seems less effective than usual.
- You consistently have stomach upset, diarrhea, or constipation.
- You recently started or stopped a medication that affects digestion.
- You are taking supplements or herbal products along with prescription medications.
- You have been diagnosed with a gastrointestinal condition.
Your provider can help you understand how these changes may influence your medication plan and whether adjustments are needed.
Supporting Gut Health for Better Medication Absorption
Maintaining a healthy digestive system can support consistent medication absorption.1 General habits that may help include eating a balanced diet rich in fiber, healthy fats, and lean proteins, and incorporating fermented foods or discussing probiotics with your healthcare provider.24 Staying well hydrated, limiting excessive alcohol and processed foods, and managing stress through calming routines can also benefit gut health.23 Additionally, avoiding the unnecessary overuse of medications that may irritate the digestive tract and following your prescription’s timing instructions exactly as directed can make a meaningful difference.1,21 While these habits are not a substitute for medical advice, they can help create a digestive environment that supports your medications working effectively.4,6,13,15
Gut health and medication absorption are closely connected. The way your stomach, intestines, and gut bacteria function can influence how well your medications work. By understanding the relationship between digestion and medication effectiveness, you can take small steps that support your treatment and improve your overall well being.13,14
If you ever have concerns about your gut health or how your body is responding to a medication, talk with your healthcare provider. With the right information and a supportive plan, you can create conditions that help your medications work their best.
References
- Brown, Marie T., and Jennifer K. Bussell. “Medication Adherence: WHO Cares?” Mayo Clinic Proceedings, vol. 86, no. 4, Apr. 2011, pp. 304–314, https://doi.org/10.4065/mcp.2010.0575.
- Ershad Sarabi, Roghayeh, et al. “The Effectiveness of Mobile Phone Text Messaging in Improving Medication Adherence for Patients with Chronic Diseases: A Systematic Review.” Iranian Red Crescent Medical Journal, vol. 18, no. 5, 30 Apr. 2016, www.ncbi.nlm.nih.gov/pmc/articles/PMC4939231/, https://doi.org/10.5812/ircmj.25183.
- Ho, P. Michael, et al. “Medication Adherence.” Circulation, vol. 119, no. 23, 16 June 2009, pp. 3028–3035, www.ahajournals.org/doi/full/10.1161/circulationaha.108.768986, https://doi.org/10.1161/circulationaha.108.768986.
- Jimmy, Benna, and Jimmy Jose. “Patient Medication Adherence: Measures in Daily Practice.” Oman Medical Journal, vol. 26, no. 3, May 2021, pp. 155–159, www.ncbi.nlm.nih.gov/pmc/articles/PMC3191684/, https://doi.org/10.5001/omj.2011.38.
- Estefanía Martínez, et al. “Oral Dosage Forms for Drug Delivery to the Colon: An Existing Gap between Research and Commercial Applications.” Journal of Materials Science Materials in Medicine, vol. 36, no. 1, 5 Mar. 2025, https://doi.org/10.1007/s10856-025-06868-5.
- Johns Hopkins Medicine. “Help for Managing Multiple Medications.” Www.hopkinsmedicine.org, 2024, www.hopkinsmedicine.org/health/wellness-and-prevention/help-for-managing-multiple-medications.
- Olsson, Regan. “The Importance of Taking Medications as Prescribed | Banner.” Www.bannerhealth.com, 4 Mar. 2021, www.bannerhealth.com/healthcareblog/teach-me/the-importance-of-taking-your-medication-as-prescribed.
- Religioni, Urszula , et al. “Enhancing Therapy Adherence: Impact on Clinical Outcomes, Healthcare Costs, and Patient Quality of Life.” Medicina, vol. 61, no. 1, 17 Jan. 2025, pp. 153–153, pmc.ncbi.nlm.nih.gov/articles/PMC11766829/, https://doi.org/10.3390/medicina61010153.
- Tariq, Rayhan, et al. “Medication Dispensing Errors and Prevention.” National Library of Medicine, StatPearls Publishing, 2024, www.ncbi.nlm.nih.gov/books/NBK519065/.