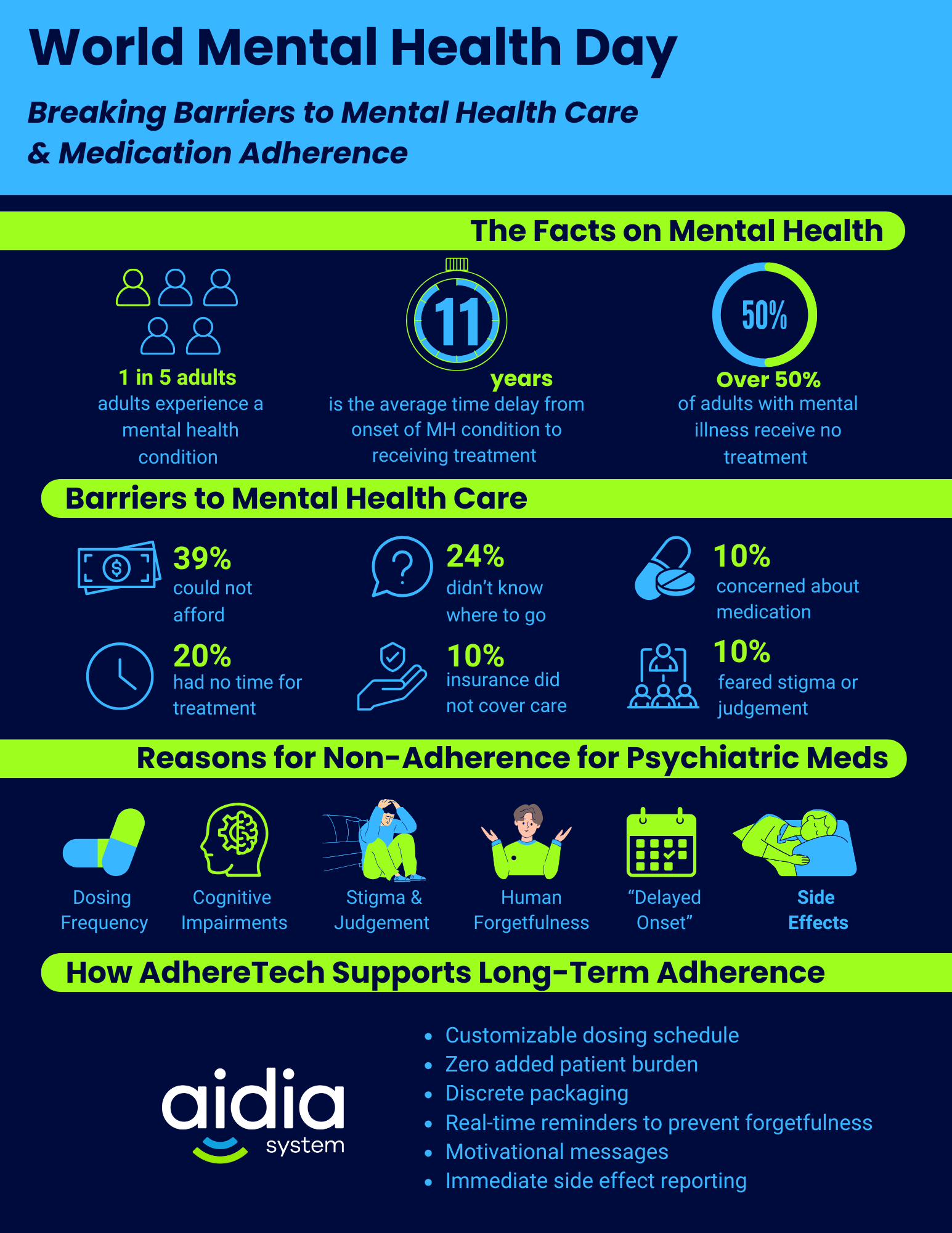
In the United States, every one in five adults experiences a mental illness.1
Prevalence of Mental Disorders:1
- 19.1% of Americans are diagnosed with an anxiety disorder(s).
- 8.3% of Americans experience a major depressive episode(s).
- 3.6% of Americans are diagnosed with PTSD.
- 2.8% of Americans are living with bipolar disorder, including types I and II.
- 1.4% of Americans are diagnosed with borderline personality disorder.
- 1.2% of Americans are living with obsessive compulsive disorder.
- 1% of Americans are diagnosed with a schizophrenia spectrum disorder.
Despite the prevalence of mental conditions within American society, the average delay between onset of a mental health disorder and treatment is an estimated 11 years.1 As a result, more than 50% of adults with a mental health condition reported not receiving treatment.1 Although the inherent nature of certain conditions may deter individuals from seeking out treatment, a series of societal barriers play a substantial role in preventing individuals from accessing the services they need to effectively manage their condition. A national survey from the U.S. The Department of Health and Human Services reported the prevalence of the following reasons for Americans not receiving mental health services within the prior year …
- 39% could not afford costs.2
- 24% did not know where to go to receive treatment.2
- 20% did not feel they had the time to seek out and receive treatment.2
- 16% did not have insurance that provided enough coverage for mental health services.2
- 12% shared concerns about committing to and/or having to take medications for their condition.2
- 10% reported fears of neighbors or members of their community having a negative reaction to their condition.2
Individuals’ willingness and ability to seek out mental health services are also significantly impacted by demographic variables. One’s race/ethnicity, sex, socioeconomic status, location, and the intersection of these attributes result in significant disparities in care.
Race/Ethnicity
While the prevalence of mental disorders appear to be higher among White Americans than Black and Hispanic Americans, this may be attributed to the inherent accessibility of mental health services for these individuals, resulting in an increased likelihood of their condition(s) going undiagnosed.3 For instance, White Americans are far more likely to report receiving mental health services within the past three years (50%), compared with 39% of Black and 36% of Hispanic Americans.4 Marginalized racial groups reported disproportionate challenges with finding a provider who understood their background and experience, lacking information to access care, and stigma or feelings of embarrassment in seeking out psychological services.4
Additionally, disproportionate health coverage across racial and ethnic groups within America may also play a role in the reduced likelihood of diagnosis and treatment. While 73.7% of White Americans have employer/private insurance, only 52.1% of Black and 48.8% of Hispanic Americans have this form of coverage.5 Meanwhile, rates of uninsurance, 17.9% for Hispanic and 9.7% for Black Americans, are higher than those of their White counterparts, which are reportedly driven by lower rates of private insurance coverage.5 While individuals with good insurance coverage plans may have co-pays as low as $0, for those without insurance, the average cost of therapeutic and psychiatric services are an estimated $100-300 and $100-500 (excluding medication costs) per session.6 With 20.6% of Black and 16.6% of Hispanic Americans living below the poverty line, even with partial coverage, the cost associated with accessing such services are prohibitive.7
While free, virtual support services are available, such as the 988 hotline – a mental health crisis line which provides emotional support, crisis management, and referrals to short and long-term resources – knowledge of its existence remains low across racial groups throughout the United States.4 However, knowledge is not equal across all Americans, with Black (16%) and Hispanic (11%) populations being far less likely to know of such service’s existence when compared to their White counterparts.4
Sex
Research consistently highlights that men are significantly less likely to seek out help for their mental health than women.8 In America, many argue that society expects men to exhibit the “Marlboro man ideal,” which entails men presenting as tough, independent, and unemotional.8 For counseling services to be beneficial, men must admit they need help, rely on a counselor, and explore their emotions – all of which directly contradict the traditional ideals associated with being a “man.”8 Similarly, social norms also play a role, with many men feeling societal pressure to “tough out” their issues on their own and experiencing fear that society will look down on them if they are unable to fix their problems independently.
While the definition of “masculinity” varies across cultures, the underlying premise of emotional suppression persists across different cultural contexts.8 For instance, a diagnosis of depression is frequently considered as incompatible with this definition as the symptoms are often referred to as feminine emotional experiences.8 Unfortunately, this ideology contributes to men being conditioned to seek less help, particularly for mental health services.8
Rural Areas
For those living in rural, as opposed to metropolitan and suburban areas, reduced access to providers, limited availability of speciality care providers, underutilization of existing services, and a lack of trained mental health professionals all increase their difficulty in accessing appropriate care.9 In fact, 60% of Americans live in rural areas where there are designated mental health provider shortages, and a staggering 65% of nonmetropolitan counties do not have any available psychiatrists.9 This lack of providers likely contributes to workplace insurance in rural areas often not covering mental health benefits or imposing stringent limitations on service accessibility, adding additional, unnecessary costs to patients that limit their ability to receive treatment.9
Similarly, the increased risk of poverty and childhood exposure to teratogens (substances or agents that can cause developmental abnormalities in growing fetuses) in rural communities may explain the heightened prevalence of mental, behavioral, and developmental disorders among children in small, non-metropolitan areas.9 Unfortunately, the dire shortage of mental health specialists trained in childhood and adolescent care within these areas often results in these conditions going untreated.9
With rural communities often lacking mental health providers many patients are forced to travel extensive distances to receive treatment.9 This introduces a series of barriers, such as the need to request time off from work, transportation costs, costs associated with of childcare and time-off from work, and frequently, a lack of transportation options to attend such appointments unless individuals have access to a car.9
When considering the intersection of race and rural locations, the prevalence of mental distress is higher among racial and ethnic minorities in rural areas than among non-hispanic Whites.9 This is particularly concerning considering that these groups are more likely to experience persistent unemployment and poverty.9 Lengthy travel distances and the costs associated with accessing mental health services without insurance disproportionately impact these communities, resulting in significantly reduced rates of treatment.9 These disparities are further amplified among individuals of marginalized racial groups living in rural areas who express high levels of mistrust in the American healthcare system and low acceptance of psychological and psychiatric services.5
Unfortunately, the slew of barriers preventing individuals from accessing mental health services likely contributes to reported suicide rates being nearly double of those in urban areas.9 Geographical isolation, greater access to lethal means, and a culture that prioritizes individualism and self-dependance may all enhance stigma around seeking out or receiving services for mental illness, particularly suicidality.9 Notably, over 25% of veterans are reported to be living in rural areas.9 Despite one in every four American veterans meeting the diagnostic criteria for a mental health condition, 5% higher than the national average – stigma, financial challenges, and issues with accessing care via the Veteran’s Association healthcare system, often prevent veterans from receiving the help they need.10 Unfortunately, these barriers to receiving care likely contribute to the heightened prevalence of suicidality in rural communities.
Reasons for Non-Adherence to Medications for Psychiatric Disorders
Medication-Related Factors
- Medication efficacy → Inadequate response to treatment, even as early as two weeks into initiating pharmacotherapy, is one of the most frequently cited reasons for discontinuing medication.11, 12
- Some studies suggest there is a “delayed onset” for antipsychotic medications, ranging from 2-3 weeks.13
- Additionally, some patients may notice symptom improvement after beginning their medication, which may result in them discontinuing their medication due to “feeling better” or no longer feeling as though they need it.14
- SSRIs often require consistent adherence for 6-8 weeks before patients begin to see improvements in their symptoms.15
- Some studies suggest there is a “delayed onset” for antipsychotic medications, ranging from 2-3 weeks.13
- Dosing Frequency → More complex dosing regimens are associated with lower adherence.16
- Once daily = 20% non-adherence17
- Twice daily = 30% non-adherence17
- Three times daily = 60% non-adherence17
- Four times daily = 70% non-adherence17
- Length of Treatment → Long-term treatment duration has been associated with medication non-adherence, particularly for patients on medications for 6-12+ months.14
- Mental health conditions are considered chronic conditions, frequently requiring long-term treatment adherence.
- Side Effects → Experiencing unpleasant side effects increase the risk of non-adherence.11, 12, 14
- Potential side effects of SSRIs:18
- Sexual dysfunction
- Headache
- Sleep disturbances
- Weight changes
- Worsened anxiety
- Dizziness
- Gastrointestinal issues
- Dry mouth
- Risk of suicidal thoughts or behaviors
- Serotonin syndrome → Symptoms range from mild (diarrhea and nausea) to severe (fevers and seizures).
- Antidepressant discontinuation syndrome → If someone discontinues their medication suddenly they can experience nausea, insomnia, fatigue, and muscle aches.
- Potential side effects of anti-psycotic medications:19
- Dizziness
- Weight gain
- Yellowing skin and eyes
- Heart and circulatory problems
- Painful muscle contractions
- Tremors
- Trouble staying awake
- Weakened immune system
- Gastrointestinal issues
- Changes in menstrual cycle
- Dry mouth
- Potential side effects of SSRIs:18
- Many of these side effects from medications used to treat psychiatric disorders can impair one’s ability to establish and maintain a consistent daily routine.
- For instance, consider the sleep disturbances from medications that can cause insomnia, fatigue, and sedation. These may all disrupt an individual’s sleeping habits, such as increasing or decreasing sleep duration, which can result in variable waking-sleeping cycles. If an individual is required to take their medications upon awakening or before falling asleep, the irregularity of these sleep-wake patterns can make it exceptionally challenging to take medications within their intended dosing windows.
- Likewise, additional side effects, such as nausea, dizziness, or appetite changes, can interfere with daily routines and further complicate sustained adherence. When patients experience unpredictable fluctuations in how they feel or function, maintaining consistent medication-taking behaviors becomes even more challenging.
- Over time, this inconsistency can lead to missed or delayed doses, compromising treatment effectiveness and increasing symptom instability. In psychiatric conditions where symptom control depends on maintaining steady medication levels, such disruptions can create a feedback loop, where medication side effects disrupt routines, and disrupted routines, in turn, worsen adherence and symptom management.
The Implications of Stigma
- Mental health conditions are the most stigmatized chronic conditions.20
- Stigma is defined as the public holding a negative view of individuals with attributes perceived by the general population as inferior, threatening, or having other negative connotations.21
- Misconceptions from the public include believing that people living with a mental illness are dangerous, incompetent, responsible for their condition, and/or unpredictable.20 This can result in a reluctance from individuals to seek out treatment due to fears of being viewed poorly by others, experiencing job and housing discrimination, and becoming rejected by society.20
- Stigma is defined as the public holding a negative view of individuals with attributes perceived by the general population as inferior, threatening, or having other negative connotations.21
- Self-stigma
- The gradual process in which a person (e.g. a psychiatric patient) adopts the negative societal views and prejudices others hold about their condition, internalizing them so that they view others’ perceptions as fact.21
- Higher self-stigma is associated with lower levels of adherence and a reluctance to seek out help/treatment across psychiatric conditions.20, 21
- Ex: A study of 322 psychiatric patients across a spectrum of psychiatric diagnoses found that level of self-stigma was associated with both current adherence to treatment and discontinuation of medication in the past without psychiatrists’ recommendation.21
- Higher self-stigma is associated with lower levels of adherence and a reluctance to seek out help/treatment across psychiatric conditions.20, 21
- The gradual process in which a person (e.g. a psychiatric patient) adopts the negative societal views and prejudices others hold about their condition, internalizing them so that they view others’ perceptions as fact.21
- Familial Stigma
- Family members providing support for loved ones with mental illness may experience stigma, becoming fearful that people will blame them for their loved one’s condition or becoming socially rejected as an entire family due to their loved one’s condition.20 This stigma can lead to reductions in emotional support, increases in social isolation, and a reluctance to seek care for their loved one(s).20
- A lack of social support has been associated with reduced treatment adherence and recovery outcomes for those living with a mental health condition.23
- Family members providing support for loved ones with mental illness may experience stigma, becoming fearful that people will blame them for their loved one’s condition or becoming socially rejected as an entire family due to their loved one’s condition.20 This stigma can lead to reductions in emotional support, increases in social isolation, and a reluctance to seek care for their loved one(s).20
- Provider-Related Stigma
- Stigma from providers toward mental health patients is common.
- Numerous patients report feeling “devalued, dismissed, and dehumanized” by the providers they encountered.24
- The most stigmatized mental health conditions include schizophrenia, BPD, and substance abuse disorders, evidenced by the dehumanizing terms frequently used to describe individuals with these disorders. Each of these terms is inappropriate, and suggests that the individual’s identity is defined by their diagnosis.24
- Therapeutic Pessimism → Providers may hold pessimistic views toward psychiatric patients’ ability to achieve recovery.25
- Relationships exist between pessimistic views of recovery and a sense of helplessness, leading some providers to believe that whatever a patient does will not matter.25
- Stigma from providers toward mental health patients is common.
Patient-Related Factors
- Lack of Insight (Anosognosia) → A condition that causes individuals to be unable to recognize they have a disorder. Individuals with anosognosia are less likely to take their medication as they do not believe they need medication.26
Prevalence:
- 50-98% of people living with a schizophrenia-spectrum disorder.27
- 40% of people living with bipolar disorder.27
- Cognitive Impairments → Mental health conditions can lead to cognitive impairments in brain areas that play a role in an individual’s attention, memory, and ability to process information – all of which increase the difficulty of patients managing their medications.26
Innate Attribute of Human Forgetfulness
While the inherent nature of psychiatric disorders and medications prescribed to treat them pose significant barriers to adherence, human nature also plays a role.
- Notably, humans across age groups all experience natural lapses and distortions in memory.29 This is due to humans having natural memory issues that may reduce medication adherence …
- Absentmindedness → Occurs when an individual does not pay close enough attention to remember something, such as the need to take their medication or whether they took their medication or not.28
- Misattribution → Occurs when an individual remembers something that is partially accurate, but misattributes a particular detail, such as the timing or day they took their medication.28
- Suggestibility → Information that you learn after an occurrence becomes incorporated into an individual’s memory, altering their memory.28 For example, reading an article on the importance of medication adherence and then that individual believing they took their medication that morning, even if they did not.29
- Persistence → Some people may experience negative distortions of reality if they persistently experience negative feelings or fears regarding a particular event.28 For instance, if a patient experienced an ADR from a different medication, they may believe they may become fearful and believe that it is definitive that they will experience adverse effects from all medications.28
- Forgetfulness has been reported to be among the highest reasons for non-adherence to psychotropic medications.29
- The combination of natural memory lapses and the cognitive impairments associated with psychiatric disorders, such as difficulties with attention, memory, and processing information,26 can make it exceptionally difficult for patients to establish and maintain consistent routines.
Breaking Barriers to Support Long-Term Consistent Medication Adherence & Patient Outcomes
Evidently, numerous barriers exist to achieving medication adherence among psychiatric patient populations. Demographic variables, the nature of various mental conditions and psychotropic medications, stigma, and inherent human nature all create challenges that can make seeking out treatment and consistent medication adherence increasingly difficult. However, effective solutions can be used to overcome these barriers, fostering psychiatric patients’ recovery and well-being.
Enhancing Cultural Competency within Healthcare
- Culturally competent care helps to facilitate communication with diverse patient populations by accounting for each patient’s cultural background, including potential language barriers and differing cultural norms that may influence treatment.30
- Examples: Tailoring communication to ensure patients understand treatment plans, potential side effects, and instructions on medication regimens.30
- Patients from diverse backgrounds may have different beliefs about mental illnesses and treatment approaches, which can reduce their willingness to remain adherent.30 Providers should work to understand and address these beliefs, ensuring they tailor treatment plans to respect patients’ personal and cultural values; this has been associated with increased medication adherence.30
- Providers should ensure that patients feel that their culture is understood and respected by their healthcare providers.30 This helps to re-establish marginalized patient populations’ trust in the healthcare system, subsequently enhancing adherence.30
- Systematic changes should address health disparities for marginalized groups, ensuring patients from all cultural backgrounds have access to quality care.30
AdhereTech: By providing real-time adherence data, AdhereTech empowers providers to see how cultural or personal factors may influence adherence and adjust dosing schedules or interventions to fit each patient’s unique context. In addition, the reminder system can be personalized—including delivery in multiple languages—ensuring that communication respects patients’ cultural values and language needs. This combination fosters trust, clarity, and more culturally responsive care.
Expanding Accessibility to Mental Health Care and Adherence Monitoring Solutions
- Utilizing digital technologies can increase accessibility to healthcare services, minimizing the need for individuals to find childcare coverage, transportation, take time off from work, etc. Findings from a scoping review indicate that the advantages of implementing digital technologies among patient populations residing in rural areas with limited access to healthcare included:
*** However, it is important to note that addressing limited internet connectivity and digital/technological literacy is essential for ensuring equitable access.
- Financial strain disproportionately impacts individuals taking psychiatric medications, increasing the risk of non-adherence.32
- Systematic changes should include the expansion of health insurance coverage and funding for existing services to address cost-related barriers to mental health treatment.32
AdhereTech: AdhereTech’s smart devices automatically collect and transmit adherence data, reducing patient burden by enabling providers to remotely monitor and support patients from the comfort of their own home. Each device comes pre-charged with a six-month battery life and connects via the global 4G network, requiring no patient setup, Wi-Fi, or smartphone access. This design directly addresses digital inequities by removing technological barriers. In addition, AdhereTech’s support team is available 7 days a week to answer patient questions and connect them with financial resources, helping ensure consistent medication coverage and long-term treatment success.
Minimizing Stigma Against Individuals Living With a Mental Health Condition
- Public awareness campaigns provide accurate information regarding mental health conditions, the prevalence of mental health disorders, and promote the possibilities for recovery.33
- Providing psychoeducation to patients and families can help to mitigate self and familial stigma regarding psychiatric disorders and medications.34
- Increasing peer support groups and recovery mentors has been shown to minimize patients’ self-stigma regarding their disorder and medication.34
AdhereTech: AdhereTech’s reminder system is grounded in behavioral psychology, providing supportive medication reminders, encouraging messages for continued adherence, and access to the company’s support team 7 days a week. The devices also include a caregiver feature, giving an extra layer of support by notifying caregivers when doses are taken or missed. Furthermore, the device’s discrete design, resembling a standard pill bottle without a medication label, protects patients’ privacy in public settings, allowing them to carry their medication without fear of judgement due to their standard bottle’s label. This approach normalizes medication management, reduces self-stigma, and helps patients feel supported in taking their medication rather than judged, fostering a more positive relationship with their treatment.
How AdhereTech Addresses Additional Barriers to Foster Prolonged Adherence
Measuring Medication Efficacy and Tailoring Treatment Regimens:
- AdhereTech’s smart devices provide real-time adherence data, allowing clinicians to quickly see whether patients are following their regimen. This data helps distinguish between non-response due to non-adherence versus true lack of efficacy, leading to more accurate treatment decisions and faster paths to recovery.
Immediate Reporting of Adverse Events:
- AdhereTech allows for immediate reporting of adverse events linked to missed doses or interruptions in adherence. For example, if adherence suddenly drops, providers can quickly check for tolerability issues and adjust treatment before patients disengage. This real-time feedback loop improves safety and strengthens trust between patients and providers.
Addressing Human Forgetfulness and Cognitive Impairments
- AdhereTech directly addresses cognitive impairments and reduces forgetfulness, through an escalating reminder system. An hour before a patient’s dosing window, the device emits a gentle glow, once a patient’s dosing window, the device gently chimes every 15 minutes until it is opened or the patient’s dosing window ends. If a patient does not take their medication within their dosing window, they receive an SMS allowing them to select or explain their reason for missing their dose, with the ability for caregivers to receive such notifications as well. This series of reminders helps to prevent memory lapses regarding adherence and provides additional reassurance to patients regarding whether or not they took their medication.
Promotion of Long-Term Adherence
Research suggests that it takes an average of 66 days to form a new habit. While missing one opportunity to perform an action does not appear to significantly impact habit formation, but for those who engaged in consistent inconsistency, did not achieve successful habit formation.35 Over time, research indicates that this action will become more habitual.35
- AdhereTech has built its system to support this process by providing daily reminders, real-time adherence tracking, and ongoing feedback. By consistently prompting patients to take their medication and providing immediate reinforcement when doses are taken, AdhereTech helps transform medication-taking from a conscious effort into a reliable daily habit, increasing long-term adherence and improving treatment outcomes.
References
1 National Alliance on Mental Illness. (2023, April). Mental health by the numbers. National Alliance on Mental Illness. Retrieved October 3, 2025, from https://www.nami.org/about-mental-illness/mental-health-by-the-numbers/
2 Controy, J., Lin, L., & Ghaness, A. (2020, July 1). Why people aren’t getting the care they need. Monitor on Psychology, 51(5). Retrieved October 3, 2025, from https://www.apa.org/monitor/2020/07/datapoint-care
3 American Psychiatric Association. (2017, December 19). Mental health facts for diverse populations. https://www.psychiatry.org/getmedia/bac9c998-5b2d-4ffa-ace9-d35844b8475a/Mental-Health-Facts-for-Diverse-Populations.pdf
4 Panchal, N., Hill, L., Artiga, S., & Hamel, L. (2024, May 23). Racial and ethnic disparities in mental health care: Findings from the KFF survey of racism, discrimination and health. Kaiser Family Foundation. https://www.kff.org/racial-equity-and-health-policy/racial-and-ethnic-disparities-in-mental-health-care-findings-from-the-kff-survey-of-racism-discrimination-and-health/
5 Hill, L., Ndugga, N., Artiga, S., & Damico, A. (2025, February 13). Health coverage by race and ethnicity, 2010–2023. Kaiser Family Foundation. https://www.kff.org/racial-equity-and-health-policy/health-coverage-by-race-and-ethnicity/
6 Doctor On Demand. (n.d.). Cost & insurance. Retrieved October 3, 2025, from https://doctorondemand.com/about-us/cost-insurance/
7 Kaiser Family Foundation. (2023). Poverty rate by race/ethnicity. Retrieved October 3, 2025, from https://www.kff.org/state-health-policy-data/state-indicator/poverty-rate-by-raceethnicity/
8 Winerman, L. (2005, June). Helping men to help themselves. Monitor on Psychology, 36(6). Retrieved October 3, 2025, from https://www.apa.org/monitor/jun05/helping
9 Morales, D. A., Barksdale, C. L., & Beckel-Mitchener, A. C. (2020). A call to action to address rural mental health disparities. Journal of Clinical and Translational Science, 4(5), 463–467. doi:10.1017/cts.2020.42
10 Charlie Health Editorial Team & Gasparini, D. (2024, February 1). 7 alarming veternal mental health statistics (and tips for support). Charles Health. https://www.charliehealth.com/research/veteran-mental-health-statistics#:~:text=Active%20military%20service%20lasts%20for,for%20SUD%20also%20have%20PTSD.
11 Kane, J. M., Kishimoto, T., & Correll, C. U. (2013). Non-adherence to medication in patients with psychotic disorders: epidemiology, contributing factors and management strategies. World psychiatry : official journal of the World Psychiatric Association (WPA), 12(3), 216–226. https://doi.org/10.1002/wps.20060
12 Marasine, N. R., & Sankhi, S. (2021). Factors Associated with Antidepressant Medication Non-adherence. Turkish journal of pharmaceutical sciences, 18(2), 242–249. https://doi.org/10.4274/tjps.galenos.2020.49799
13 Kapur, S., Arenovich, T., Agid, O., Zipursky, R., Lindborg, S., & Jones, B. (2005). Evidence for onset of antipsychotic effects within the first 24 hours of treatment. American Journal of Psychiatry, 162(5), 939–946. https://doi.org/10.1176/appi.ajp.162.5.939
14 Semahegn, A., Torpey, K., Manu, A., Assefa, N., Tesfaye, G., & Ankomah, A. (2020). Psychotropic medication non-adherence and its associated factors among patients with major psychiatric disorders: a systematic review and meta-analysis. Systematic reviews, 9(1), 17. https://doi.org/10.1186/s13643-020-1274-3
15 Smedley, T., & Murdock, J. (2025, July 29). How long does it take for antidepressants to start working? GoodRx. https://www.goodrx.com/conditions/depression/time-for-antidepressants-to-work
16 Malik, M., & Kumari, S. (2020, March 27). Treatment nonadherence: An epidemic hidden in plain sight. Psychiatric Times 37(3). https://www.psychiatrictimes.com/view/treatment-nonadherence-epidemic-hidden-plain-sight
17 Aljofan, M., Oshibayeva, A., Moldaliyev, I., Saruarov, Y., Maulenkul, T., & Gaipov, A. (2023). The rate of medication nonadherence and influencing factors: A systematic Review. Electronic Journal of General Medicine, 20(3).
18 Cleveland Clinic. (2025, October 3). SSRIs (Selective serotonin reuptake inhibitors). https://my.clevelandclinic.org/health/treatments/24795-ssri
19 Cleveland Clinic. (2023, October 3). Antipsychotic medications: What they are, uses & side effects. https://my.clevelandclinic.org/health/treatments/24692-antipsychotic-medications
20 American Psychiatric Association. (n.d.). Stigma, prejudice and discrimination against people with mental illness. Retrieved October 3, 2025, from https://www.psychiatry.org/patients-families/stigma-and-discrimination
21 Kamaradova, D., Latalova, K., Prasko, J., Kubinek, R., Vrbova, K., Mainerova, B., Cinculova, A., Ociskova, M., Holubova, M., Smoldasova, J., & Tichackova, A. (2016). Connection between self-stigma, adherence to treatment, and discontinuation of medication. Patient preference and adherence, 10, 1289–1298. https://doi.org/10.2147/PPA.S99136
22 Kapur, S., Arenovich, T., Agid, O., Zipursky, R., Lindborg, S., & Jones, B. (2012). Evidence for onset of antipsychotic effects within the first 24 hours of treatment. American Journal of Psychiatry, 162(5), 939–946. https://doi.org/10.1176/appi.ajp.162.5.939
23 Scheurer, D., Choudhry, N., Santon, K., Matlin, O., & Shrank, W. (2012). Association between different types of social support and medication adherence. The American Journal of Managed Care 18(12). https://scholar.harvard.edu/files/nkc/files/2012_social_supports_medication_adherence_ajmc.pdf
24 American Psychological Association. (2024, July). Fighting stigma by mental health providers toward patients. Monitor on Psychology. https://www.apa.org/monitor/2024/07/stigma-against-patients
25 Gunasekaran, S., Tan, G. T. H., Shahwan, S., Goh, C. M. J., Ong, W. J., & Subramaniam, M. (2022). The perspectives of healthcare professionals in mental health settings on stigma and recovery – A qualitative inquiry. BMC health services research, 22(1), 888. https://doi.org/10.1186/s12913-022-08248-z
26 Boyer, L., Cermolacce, M., Dassa, D., Fernandez, J., Boucekine, M., Richieri, R., Vaillant, F., Dumas, R., Auquier, P., & Lancon, C. (2012). Neurocognition, insight and medication nonadherence in schizophrenia: a structural equation modeling approach. PloS one, 7(10), e47655. https://doi.org/10.1371/journal.pone.0047655
27 Cleveland Clinic. (2022, October 3). Anosognosia: What it is, causes, symptoms & treatment. https://my.clevelandclinic.org/health/diseases/22832-anosognosia
28 Harvard Health Publishing. (2021, February 12). Forgetfulness – 7 types of normal memory problems. Harvard Health Publishing. https://www.health.harvard.edu/mind-and-mood/forgetfulness-7-types-of-normal-memory-problems
29 Bulloch, A. G., & Patten, S. B. (2010). Non-adherence with psychotropic medications in the general population. Social psychiatry and psychiatric epidemiology, 45(1), 47–56. https://doi.org/10.1007/s00127-009-0041-5
30 Raza, M. A., Aziz, S., Iftikhar, D., Anjum, I., & Fialova, D. (2024). Addressing quality medication use among migrant patients: Establishment of an organization to provide culturally competent medication care. Saudi Pharmaceutical Journal, 32(3), 101922. https://doi.org/10.1016/j.jsps.2024.101922
31 Maita, K. C., Maniaci, M. J., Haider, C. R., Avila, F. R., Torres-Guzman, R. A., Borna, S., Lunde, J. J., Coffey, J. D., Demaerschalk, B. M., & Forte, A. J. (2024). The Impact of Digital Health Solutions on Bridging the Health Care Gap in Rural Areas: A Scoping Review. The Permanente journal, 28(3), 130–143. https://doi.org/10.7812/TPP/23.134
32 Stickland, J., Stoops, W., Kincer, M., & Rush, C. (2019, January). The impact of financial strain on medication non-adherence: Influence of psychiatric medication use. Psychiatry Research 271, 389-395. https://doi.org/10.1016/j.psychres.2018.11.055
33 Ahad, A. A., Sanchez-Gonzalez, M., & Junquera, P. (2023). Understanding and Addressing Mental Health Stigma Across Cultures for Improving Psychiatric Care: A Narrative Review. Cureus, 15(5), e39549. https://doi.org/10.7759/cureus.39549
34 Laranjeira, C., Carvalho, D., Valentim, O., Moutinho, L., Morgado, T., Tomás, C., Gomes, J., & Querido, A. (2023). Therapeutic Adherence of People with Mental Disorders: An Evolutionary Concept Analysis. International journal of environmental research and public health, 20(5), 3869. https://doi.org/10.3390/ijerph20053869
35 University College of London. (2009, August 4). How long does it take to form a habit?. https://www.ucl.ac.uk/prospective-students