How to Empower Medication Success for Someone You Love
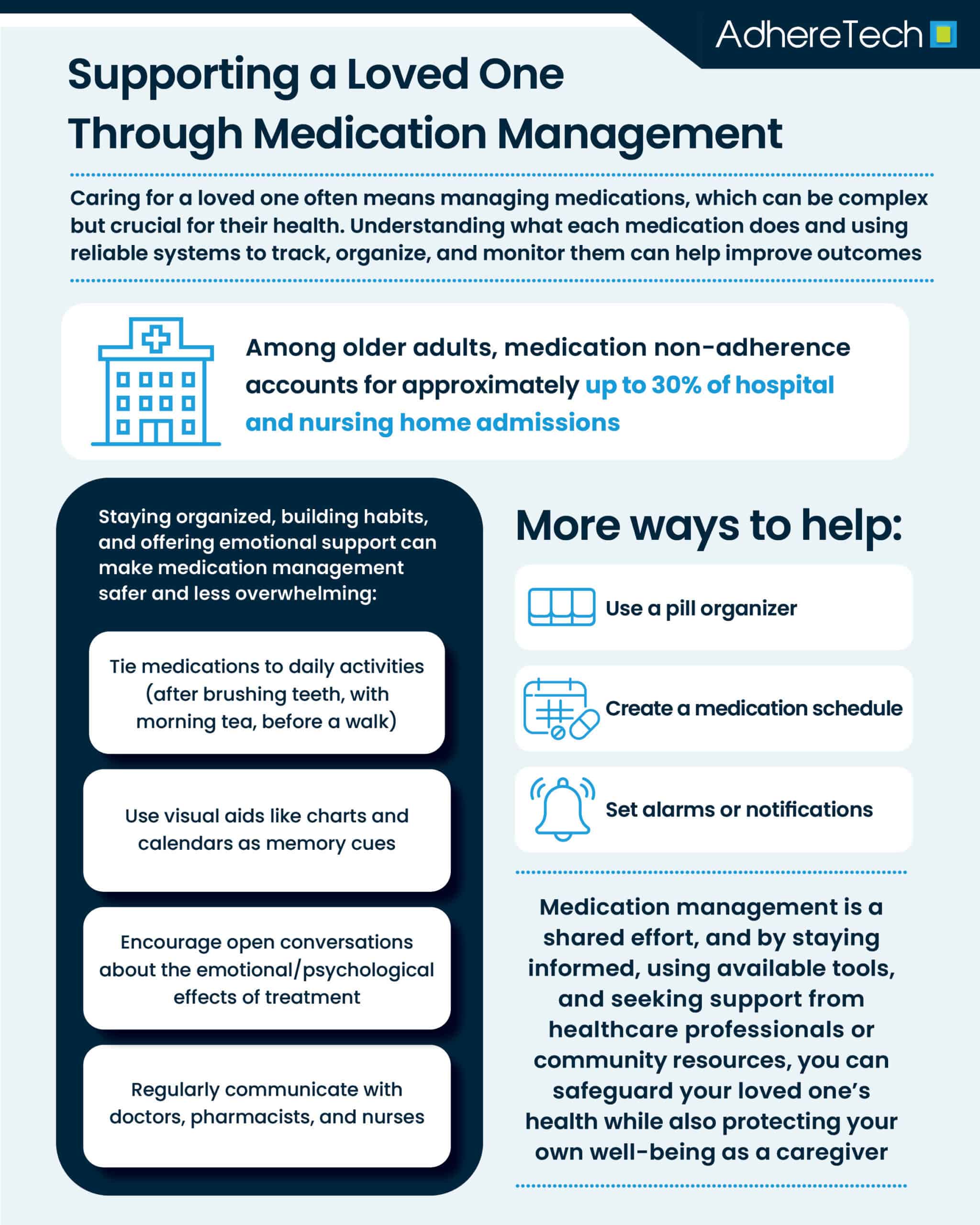
Caring for a loved one often involves a wide range of responsibilities, and medication management can be one of the most crucial and complex. Whether your loved one is aging, recovering from surgery, or managing a chronic condition, ensuring that medications are taken correctly and safely can significantly impact their health outcomes. Among older adults, medication non-adherence accounts for approximately up to 30% of hospital and nursing home admissions.1
Understanding the Importance of Medication Management
Medication adherence, which means taking medications exactly as prescribed by a healthcare provider, is vital for treating and managing many medical conditions.2 For older adults, medication mismanagement can contribute to falls, hospital readmissions, and cognitive decline.3
Understanding the medications your loved one is taking, including their purpose, dosage, potential side effects, and interactions, is the first step to providing effective support. Being informed allows caregivers to assist with organizing medications, tracking usage, and spotting potential problems before they escalate.
Organizing Medications Effectively
Disorganization is a common cause of missed doses and medication errors.4 Creating a reliable medication system can prevent confusion and ensure treatment consistency. Here are a few ways to help:
- Use a Pill Organizer: Weekly or monthly pill boxes with compartments for different times of day help separate different medications and label each dose clearly.
- Create a Medication Schedule: A printed or digital chart listing each medication, dosage, timing, and special instructions makes the routine easier to follow. Some apps also provide reminders and tracking features.
- Set Alarms or Notifications: Smartphone alarms, voice assistants, or smart devices can prompt your loved one when it is time to take their medication.
These systems can help caregivers ensure correct dosing by reducing reliance on memory, promoting independence and providing a tangible reminder system. .
Involving Healthcare Professionals
Regular communication with doctors, pharmacists, and nurses is essential for successful medication management, as healthcare professionals can provide clarity about medication changes, side effects, and potential interactions.5 Keeping comprehensive documentation, including an up-to-date medication list, side effects, and concerns, and bringing it to all medical appointments helps ensure accuracy and safety. Pharmacists can be asked to review all medications to identify potential risks, especially when medications are taken in combination with over-the-counter drugs or supplements. During transitions of care, such as after a hospital discharge, requesting a medication review or reconciliation can help prevent errors and duplications.6 Pharmacists, in particular, are an underutilized resource that can simplify regimens, recommend combination medications, or prepare blister packs tailored to a patient’s specific needs.7
Building a Routine Around Medication
One effective way to improve adherence is by integrating medication into a patient’s existing daily routine, as habit formation plays a critical role in ensuring long-term consistency.8 When a task is anchored to a familiar habit — for example, taking medication immediately after brushing teeth, with a morning cup of tea, or right before a daily walk — it becomes part of the brain’s automatic sequence of behaviors, reducing the need for conscious decision-making each time.8 This “cue and response” pattern not only increases the likelihood of remembering doses but also helps create a sense of normality around treatment, making it feel like a natural part of the day rather than a disruptive chore. Routines are particularly valuable for individuals with cognitive impairments or dementia, as they provide structure and predictability, which can reduce anxiety, confusion, and frustration.9
For those with memory challenges, reinforcing the habit through visual aids (such as color-coded charts, a whiteboard calendar, or clearly labeled pill organizers) can provide additional cues and confirmation of medication taking behaviors. In more complex cases, medication management systems or home health aides can offer daily assistance, ensuring that medications are correctly dosed and taken on time. Over time, the combination of habit integration, environmental reminders, and supportive resources can significantly improve adherence, leading to better health outcomes and greater independence.10
Supporting Emotional and Psychological Wellbeing
Medication management is not just a logistical issue, it also involves emotional and psychological components. Many people feel overwhelmed by the number of medications they must take or the complexity of their medications (ex: 2+ daily dosing), especially if they are dealing with a recent diagnosis or a long-term illness. Others may feel resistant or fearful due to side effects, stigma, or a sense of lost independence.11
As a caregiver, offering emotional support and empathy is just as important as managing schedules. Encourage open conversations about how your loved one feels regarding their medication. Listen without judgment, and be patient when resistance arises. Addressing their concerns with a doctor or therapist can sometimes lead to adjustments that make the regimen more tolerable.
Motivational interviewing — a communication technique that encourages individuals to talk about their own reasons for change — can be helpful in this context.12 Rather than telling a loved one what to do, ask open-ended questions and express support for their autonomy.
Watching for Side Effects and Interactions
Side effects can be a major reason why individuals stop taking medications.11 These may include fatigue, nausea, dizziness, or mood changes.13 In older adults, side effects may be mistaken for signs of aging or illness. It is important to monitor for:14
- New or worsening symptoms
- Changes in appetite or sleep
- Mood or cognitive shifts
- Unexplained falls or confusion
Report any concerns promptly to a healthcare provider. In some cases, side effects may be managed with a change in timing, dosage, or formulation.
Managing Medications Across Different Settings
If your loved one moves between home, hospital, rehab, or assisted living, medication routines can be disrupted. During transitions of care, medication reconciliation is critical to prevent duplication, omissions, or dangerous interactions.12 Caregivers should ensure that: a complete medication list is provided to each provider, discharge instructions are reviewed thoroughly, and any new prescriptions are understood before leaving the facility. Clear communication between care teams and family members can prevent misunderstandings and ensure continuity of care.
Knowing When to Ask for Help
Managing someone else’s medication needs can be overwhelming, especially if you are balancing work, family, and your own health. Caregiver burnout is real and can impair your ability to provide safe and compassionate support.
Consider enlisting additional help when needed. Options for this may include professional in-home care services, medication management programs through local pharmacies, adult day programs or respite care, or remote medication monitoring technologies. Additionally, caregiver support groups can provide emotional support, practical advice, and a sense of community.
Supporting a loved one through medication management is a responsibility that blends practical organization, medical knowledge, and compassionate care. By taking a proactive, informed, and empathetic approach, you can help your loved one stay safe, feel supported, and maintain as much independence as possible.
Remember, you do not have to do it alone. Collaborating with healthcare professionals, using available tools, and seeking support when needed will not only improve outcomes for your loved one but also help you sustain your role as a caregiver.
References
- Mills, William R, et al. “A Novel Home-Based Medication Management Program and Its Influence on Hospitalization Rates among Home Health Care Recipients.” Journal of the American Medical Directors Association, vol. 25, no. 1, 1 Jan. 2024, pp. 155-157.e1, https://doi.org/10.1016/j.jamda.2023.10.012.
- World Health Organization (WHO). (2003). Adherence to long-term therapies: Evidence for action. World Health Organization.
- Badawy, Sherif M, et al. “Habit Strength, Medication Adherence, and Habit-Based Mobile Health Interventions across Chronic Medical Conditions: Systematic Review.” Journal of Medical Internet Research, vol. 22, no. 4, 28 Apr. 2020, p. e17883, https://doi.org/10.2196/17883.
- Barnsteiner, Jane H. “Medication Reconciliation.” Nih.gov, Agency for Healthcare Research and Quality (US), 2020, www.ncbi.nlm.nih.gov/books/NBK2648/.
- Baryakova, Tsvetelina H., et al. “Overcoming Barriers to Patient Adherence: The Case for Developing Innovative Drug Delivery Systems.” Nature Reviews Drug Discovery, vol. 22, no. 22, 27 Mar. 2023, pp. 1–23, https://doi.org/10.1038/s41573-023-00670-0.
- Burns, Leah, et al. “Real-World Evidence for Regulatory Decision-Making: Guidance from around the World.” Clinical Therapeutics, Feb. 2022, https://doi.org/10.1016/j.clinthera.2022.01.012.
- Cipriani, Gabriele, et al. “Daily Functioning and Dementia.” Dementia & Neuropsychologia, vol. 14, no. 2, 2020, pp. 93–102, pmc.ncbi.nlm.nih.gov/articles/PMC7304278/, https://doi.org/10.1590/1980-57642020dn14-020001.
- Maher, Robert L, et al. “Clinical Consequences of Polypharmacy in Elderly.” Expert Opinion on Drug Safety, vol. 13, no. 1, 27 Sept. 2014, pp. 57–65, https://doi.org/10.1517/14740338.2013.827660.
- Mardani, Abbas, et al. “The Role of the Nurse in the Management of Medicines during Transitional Care: A Systematic Review.” Journal of Multidisciplinary Healthcare, vol. 13, no. 1, 2020, pp. 1347–1361, www.ncbi.nlm.nih.gov/pmc/articles/PMC7608001/, https://doi.org/10.2147/JMDH.S276061.
- Ravi, Padma, et al. “Nurse-Pharmacist Collaborations for Promoting Medication Safety among Community-Dwelling Adults: A Scoping Review.” International Journal of Nursing Studies Advances, vol. 4, no. 4, Dec. 2022, p. 100079, pmc.ncbi.nlm.nih.gov/articles/PMC11080473/, https://doi.org/10.1016/j.ijnsa.2022.100079.
- Rollnick, S, et al. “Motivational Interviewing in Health Care: Helping Patients Change Behavior.” American Journal of Pharmaceutical Education, vol. 73, no. 7, 12 Nov. 2009, p. 127, pmc.ncbi.nlm.nih.gov/articles/PMC2779641/.
- Singh, Ben, et al. “Time to Form a Habit: A Systematic Review and Meta-Analysis of Health Behaviour Habit Formation and Its Determinants.” Healthcare, vol. 12, no. 23, 9 Dec. 2024, p. 2488, www.mdpi.com/2227-9032/12/23/2488#B5-healthcare-12-02488, https://doi.org/10.3390/healthcare12232488.
- Tariq, Rayhan, et al. “Medication Dispensing Errors and Prevention.” National Library of Medicine, StatPearls Publishing, 12 Feb. 2024, www.ncbi.nlm.nih.gov/books/NBK519065/.
- Ngcobo, Nokwanda N. “Influence of Ageing on the Pharmacodynamics and Pharmacokinetics of Chronically Administered Medicines in Geriatric Patients: A Review.” Clinical Pharmacokinetics, vol. 64, no. 1, 11 Jan. 2025, pp. 335–367, https://doi.org/10.1007/s40262-024-01466-0.