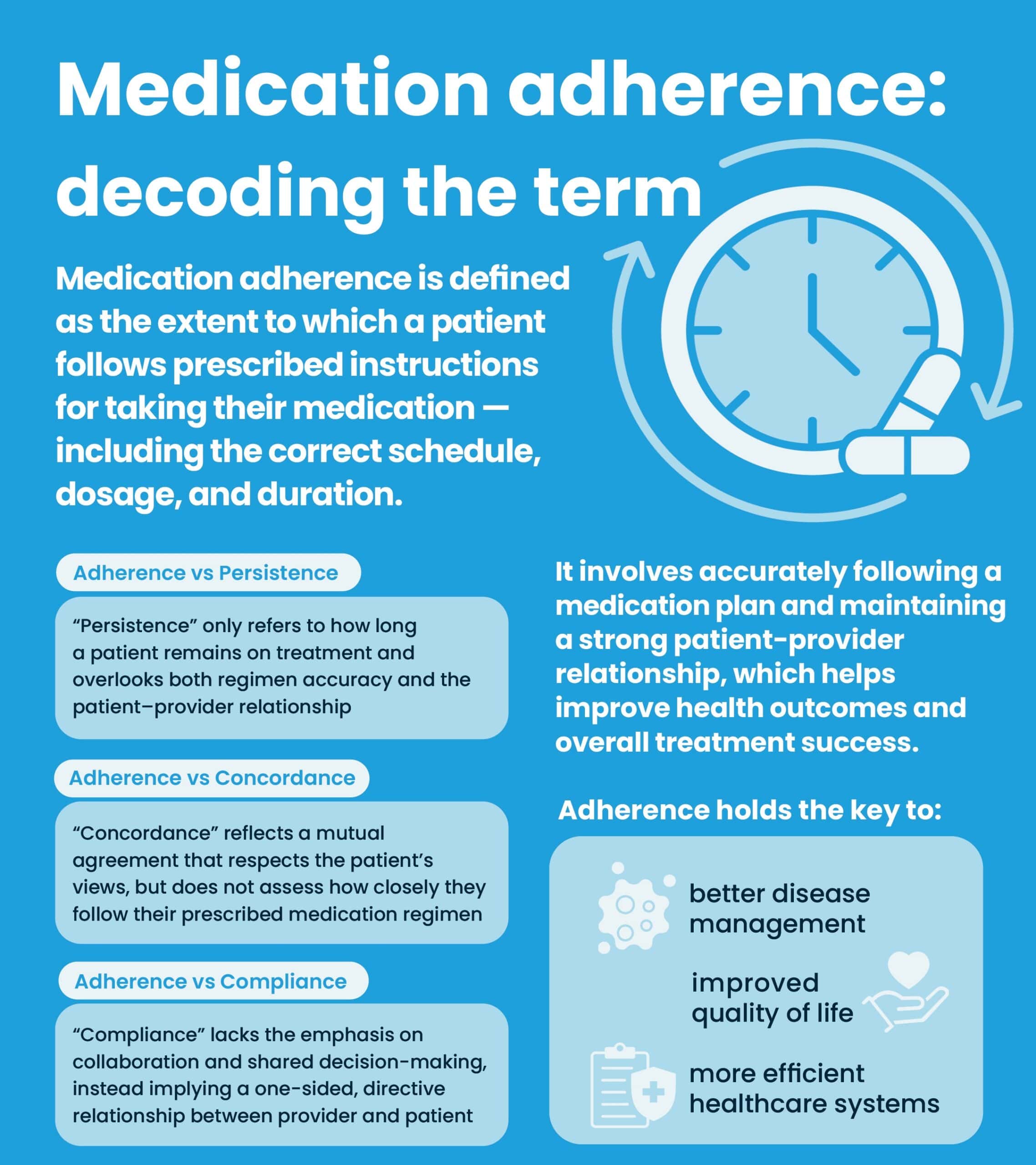
In recent years, the term medication adherence has entered the healthcare lexicon, reflecting a growing awareness of its critical role in improving health outcomes. While it may sound like a clinical term, medication adherence is something that directly affects millions of patients worldwide and holds the key to better disease management, improved quality of life, and more efficient healthcare systems1,2. Medication adherence refers to whether a patient follows the prescribed instructions for taking their medication— on the right schedule, in the right dose, and for the right duration3. The term differs slightly from compliance, which historically carried a more passive connotation, suggesting that patients simply follow orders1,3. In contrast, adherence emphasizes an active, engaged decision by patients to manage their health as prescribed1,3.
Adherence vs Persistence
Other terms that are frequently used synonymously with compliance and adherence are persistence and concordance1,3. Persistence addresses the duration a patient continues within their treatment, but does not address how accurately they follow a regimen3. Furthermore, this term neglects the relationship quality between patients and healthcare providers. These oversights can lead to a simplistic view of medication management that ignores the complexities of patient behavior and the need for a supportive healthcare relationship to achieve optimal outcomes.
Adherence vs Concordance
While concordance reflects a mutual agreement and respect for the patient’s views on their medication, it still falls short by failing to address how accurately patients follow their medication regimens4.
Adherence vs Compliance
Given compliance and adherence consider both the accuracy of a patient’s medication regimen and the relationship between healthcare providers and patients, they have become leading terms for discussing the suboptimal taking of medication by patients. However, compliance is the degree to which a patient follows a prescriber’s instructions, implying a one-way directive from doctor to patient1,4. In the clinical setting, this term makes sense, as trial participants are expected to follow the instructions they are provided. However, within the real word compliance carries a negative connotation, suggesting a one-sided relationship where the patient is expected to obey their healthcare providers without question. Therefore, in the real world, adherence has replaced compliance to emphasize a collaborative relationship between patients and healthcare providers. Adherence’s definition emphasizes this dynamic, given it proposes the extent a patient’s medication taking and execution of lifestyle changes correspond with agreed recommendations from a healthcare provider1,4.
Resultantly, medication adherence is the preferred term as it encompasses the precision of following the prescribed medication regimen and the quality of the patient-provider relationship, promoting better patient outcomes and a more holistic approach to medication management. Notably, the concept of adherence is closely related to the concept known as the therapeutic alliance, a collaborative and trusting relationship between a patient and their healthcare provider5,6. This alliance is foundational in ensuring patients feel understood and heard throughout their treatment, resulting in patients being more likely to follow through with their treatment plans7. Hence, when patients perceive their healthcare providers as partners, they are more motivated and willing to adhere to their prescribed medication regimens. Consequently, medication adherence has become the preferred term as it encompasses the precision of following the prescribed medication regimen and the quality of the patient-provider relationship, promoting better patient outcomes and a more comprehensive approach to medication management.
References
- Chakrabarti S. (2014). What’s in a name? Compliance, adherence and concordance in chronic psychiatric disorders. World Journal of Psychiatry, 4(2), 30–36. https://doi.org/10.5498/wjp.v4.i2.30.
- Bosworth, H. B., Granger, B. B., Mendys, P., Brindis, R., Burkholder, R., Czajkowski, S. M., Daniel, J. G., Ekman, I., Ho, M., Johnson, M., Kimmel, S. E., Liu, L. Z., Musaus, J., Shrank, W. H., Whalley Buono, E., Weiss, K., & Granger, C. B. (2011). Medication adherence: a call for action. American heart journal, 162(3), 412–424. https://doi.org/10.1016/j.ahj.2011.06.007
- Cramer, J. A., Roy, A., Burrell, A., Fairchild, C. J., Fuldeore, M. J., Ollendorf, D. A., & Wong, P. K. (2008). Medication compliance and persistence: terminology and definitions. Value in Health: The Journal of the International Society for Pharmacoeconomics and Outcomes Research, 11(1), 44–47. https://doi.org/10.1111/j.1524-4733.2007.00213.x
- Hugtenburg, J. G., Timmers, L., Elders, P. J., Vervloet, M., & van Dijk, L. (2013). Definitions, variants, and causes of nonadherence with medication: a challenge for tailored interventions. Patient Preference and Adherence, 7, 675–682. https://doi.org/10.2147/PPA.S29549.
- Chang, J. G., Roh, D., & Kim, C. H. (2019). Association between therapeutic alliance and adherence in outpatient schizophrenia patients. Clinical psychopharmacology and neuroscience: The Official Scientific Journal of the Korean College of Neuropsychopharmacology, 17(2), 273–278. https://doi.org/10.9758/cpn.2019.17.2.273.
- Pringle, J., & Fawcett, J. (2017). Facilitating the therapeutic alliance between pharmacists and patients to improve medication adherence. In D. S. Prescott, C. L. Maeschalck, & S. D. Miller (Eds.), Feedback-Informed Treatment in Clinical Practice: Reaching for Excellence, 299–320. American Psychological Association. https://doi.org/10.1037/0000039-016.
- Meissner, W. W. (1996). The Therapeutic Alliance. Yale University Press. http://www.jstor.org/stable/j.ctt32bj01.