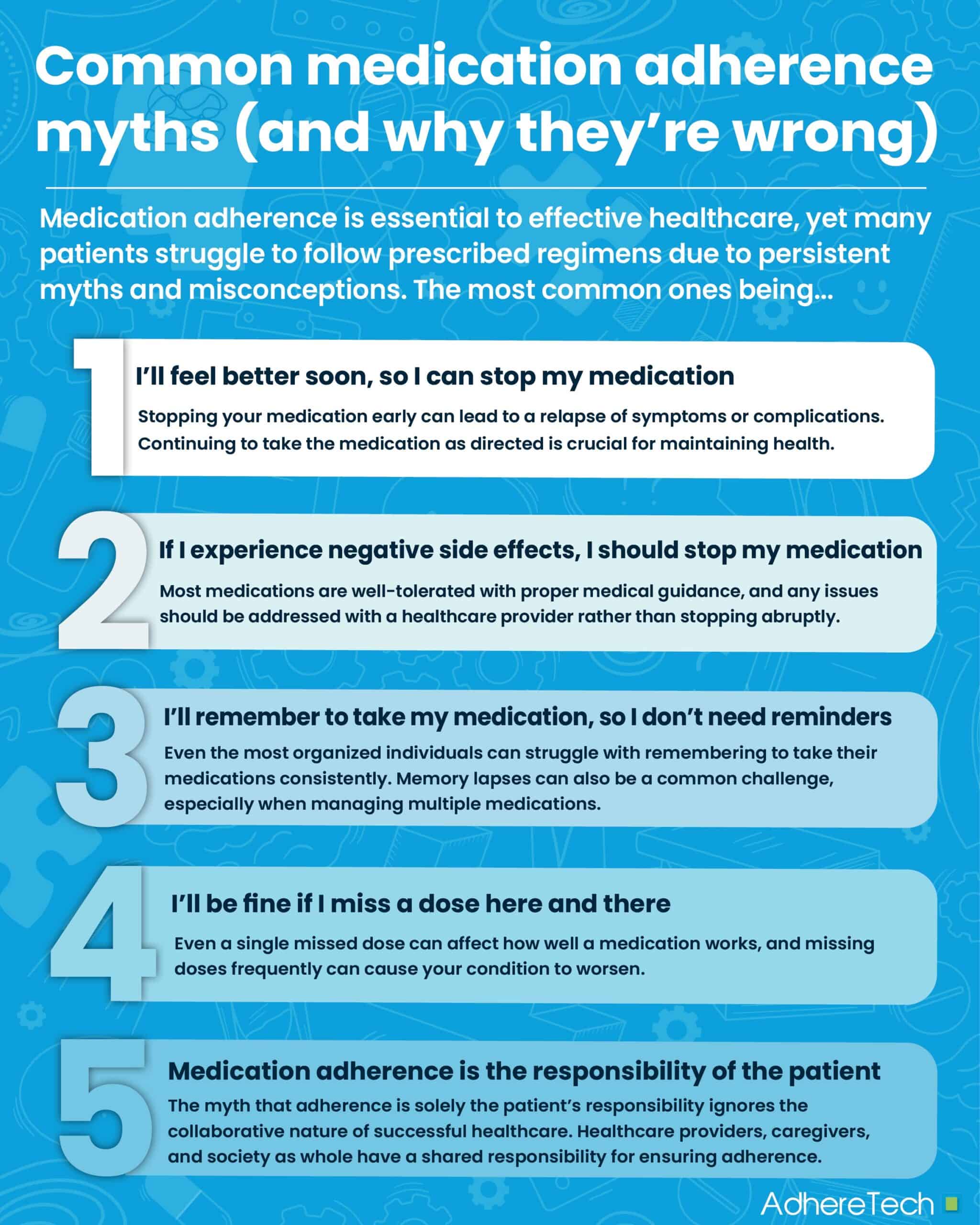
Medication adherence is a fundamental component of effective healthcare1. However, despite significant efforts to educate patients about the importance of following prescribed regimens, a large percentage of individuals still fail to adhere to their medications. According to the World Health Organization, nearly 50% of patients with chronic conditions do not take their medication as prescribed1. Non-adherence is often fueled by a series of myths and misconceptions that patients, healthcare providers, and even society hold.
“I’ll feel better soon, so I can stop my medication.”
One of the most common misconceptions is that patients can stop taking their medication once they start feeling better2. While it’s normal to feel immediate benefits from some medications (like insulin2), stopping your medication early can lead to a relapse of symptoms or complications2. For chronic conditions, like high blood pressure or diabetes, medication is typically proactive, designed to keep the condition stable and produce long-term benefits, not just treat short-term symptoms2. An example of this can be found in the case of antibiotics, where stopping treatment early can contribute to antibiotic resistance, making future infections harder to treat3. In the case of chronic conditions, such as asthma or depression, halting medication without professional guidance can result in setbacks in recovery, leading to worsened symptoms and health outcomes2.
Medications are prescribed with the intent of managing or controlling conditions in the long term, such as stabilizing blood pressure for diabetic patients or eliminating bacteria via antibiotics. Even if you feel better, continuing to take the medication as directed is crucial for maintaining health and preventing the condition from returning or worsening.
Myth 2: If I experience negative side effects, I should stop taking my medication
While some medications do have side effects, the majority of patients tolerate medications well, especially if they’re monitored and adjusted by a healthcare provider. Side effects can vary from person to person, and many can be mitigated by taking the medication at a different time of day, adjusting the dose, or switching to an alternative medication4. For example, if a patient experiences nausea with a particular drug, a doctor might recommend taking it with food or switching to a different formulation.
Stopping medication without professional advice can be extremely harmful. For instance, abruptly discontinuing antidepressants or antipsychotics can lead to withdrawal symptoms, worsening mental health, and even hospitalization5.
If you experience adverse side effects, it’s important to talk to your healthcare provider. They can make adjustments or recommend alternatives, so you don’t have to sacrifice your health.
Myth 3: “I’ll remember to take my medication, so I don’t need reminders.”
Even the most organized individuals can struggle with remembering to take their medications consistently. Life gets busy, and it’s easy to forget a dose or two, especially if you’re taking multiple medications, traveling, or attempting to balance multiple roles. Forgetting doses, even occasionally, can negatively interfere with the effectiveness of the treatment, leading to poorer health outcomes7.
Establishing new behaviors, like remembering to take medication daily, can be surprisingly challenging. It’s often said that it takes about three months of consistent effort to form a lasting habit, but only a week—or even less—to break it (depending on the individual and the complexity of the behavior)8. This is especially true with medication routines, where missing just a few days can easily disrupt the pattern, and lead to the breakdown of a newly formed behavior9. Life’s unpredictability, stress, or even minor changes in routine can cause someone to forget their dose, diminishing all the progress they’ve made. That’s why tools like reminders, pill organizers, or pairing the medication with an existing habit (like brushing your teeth) are so important—they help reinforce the behavior until it becomes second nature10.
Memory lapses are a common challenge for patients, especially when managing multiple medications11. Using reminders—whether auditory, visual, or technology-based— can significantly improve adherence. The goal is to make medication-taking a regular, seamless part of your routine.
Myth 4: “I’ll be fine if I miss a dose here and there.”
Occasional missed doses might not seem like a big deal, but missing doses on a regular basis can significantly reduce the effectiveness of your treatment plan7. The consistency of your medication regimen is what helps manage the condition over time7. Some medications, like antibiotics, require precise timing to maintain their effectiveness3, while others, such as blood thinners or insulin, have less restrictive dosing windows, but still must be taken regularly to keep conditions under control12.
Even a single missed dose can affect how well a medication works7. Missing doses too frequently can cause your condition to worsen or complicate the treatment process7. If you miss a dose, it’s important to reach out to your healthcare provider and follow your doctor’s guidance on what to do next.
Myth 5: Medication adherence is the responsibility of the patient
While patients play a key role in medication adherence, it is essential to recognize that healthcare providers, caregivers, and society at large also share responsibility for ensuring adherence. Healthcare providers must not only prescribe the correct medications but also educate patients on their treatment plans, address potential barriers to adherence, and follow up regularly to ensure that patients are on track13.
Pharmacists, too, play a critical role in improving adherence, offering guidance on medication administration, managing side effects, and reminding patients about refills13. In some cases, community support—such as family or friends assisting with medication management—can make a significant difference2. The myth that adherence is solely the patient’s responsibility ignores the collaborative nature of successful healthcare.
Medication adherence is essential for maintaining health and improving quality of life, especially for chronic conditions. Dispelling these common myths is crucial for helping patients understand the importance of following their treatment plans exactly as prescribed. If you have any concerns about your medications or how to take them, always consult with your healthcare provider. They can help clarify your doubts, provide guidance, and ensure you’re on the best path to better health.
References
- World Health Organization (WHO). (2003). Adherence to long-term therapies: Evidence for action. World Health Organization.
- Jimmy, Benna, and Jimmy Jose. “Patient Medication Adherence: Measures in Daily Practice.” Oman Medical Journal, vol. 26, no. 3, May 2021, pp. 155–159, www.ncbi.nlm.nih.gov/pmc/articles/PMC3191684/, https://doi.org/10.5001/omj.2011.38.
- NHS . “Antibiotic Resistance – Antibiotics.” NHS, 11 Nov. 2022, www.nhs.uk/conditions/antibiotics/antibiotic-antimicrobial-resistance/.
- Brazier, Yvette. “Side Effects: Medication, Types of Effect, Cancer Treatment.” Www.medicalnewstoday.com, 31 Mar. 2017, www.medicalnewstoday.com/articles/196135.
- Muench, J., & Hamer, A. M. (2010). Adherence to treatment with antipsychotic medications. Journal of Clinical Psychiatry, 71(2), 191–202. https://doi.org/10.4088/JCP.09r05088gre
- National Institute of Diabetes and Digestive and Kidney Diseases. “Diabetes, Heart Disease, and Stroke | NIDDK.” National Institute of Diabetes and Digestive and Kidney Diseases, Apr. 2021, www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/heart-disease-stroke .
- Brown, Marie T., and Jennifer K. Bussell. “Medication Adherence: WHO Cares?” Mayo Clinic Proceedings, vol. 86, no. 4, Apr. 2011, pp. 304–314, https://doi.org/10.4065/mcp.2010.0575.
- Lally, P., van Jaarsveld, C. H., Potts, H. W., & Wardle, J. (2010). How are habits formed: Modelling habit formation in the real world. European Journal of Social Psychology, 40(6), 998–1009.
- Verplanken, B., & Wood, W. (2006). Interventions to break and create consumer habits. Journal of Public Policy & Marketing, 25(1), 90–103.
- Osterberg, L., & Blaschke, T. (2005). Adherence to medication. New England Journal of Medicine, 353(5), 487–497.
- Chippa, Venu, and Kamalika Roy. “Geriatric Cognitive Decline and Polypharmacy.” PubMed, StatPearls Publishing, 2023, www.ncbi.nlm.nih.gov/books/NBK574575/.
- Mayo Clinic. “Diabetes Treatment: Using Insulin to Manage Blood Sugar.” Mayo Clinic, 4 Aug. 2023, www.mayoclinic.org/diseases-conditions/diabetes/in-depth/diabetes-treatment/art-20044084.
- DiMatteo, M. R. (2004). Variations in patients’ adherence to medical recommendations: A quantitative review of 50 years of research. Medical Care, 42(3), 200–209. https://doi.org/10.1097/01.mlr.0000114908.90348.f9
- Whelton, P. K., Carey, R. M., Aronow, W. S., et al. (2018). 2017 American College of Cardiology/American Heart Association hypertension guidelines. Hypertension, 71(6), 1269–1324. https://doi.org/10.1161/HYPERTENSIONAHA.118.12115